Non-ortho-k CL options for myopia control
Last year, I gave an account of my personal sob-story of rampant myopia and discussed how modern day orthokeratology (ortho-k) contact lenses can be modified to potentially improve their myopia control effect through smaller diameter aspheric optics. This year, I thought I would explore some of the other contact lens options that will give non-ortho-k practitioners the ability to slow myopia and decrease the risk of permanent ocular disease in their young patients.
The case for CLs
Contact lens management for myopia control continues to be the mainstay of treatment in my practice. Part of this may be to do with the patient’s and parent’s somewhat naive perspective that the primary burden of myopia - the necessity for glasses - has been solved with contact lenses! I am happy, however, because their child’s myopia is being slowed. So, really, everyone wins!
Recent questions have also been raised¹ regarding the effectiveness of low dose atropine actually slowing axial growth, rather than just affecting refractive change, as reported in the meta-analysis last year from Gong et al 2017². All further reason to use contact lenses for myopia control due to their proven effect at slowing axial length change.
Animal models, from the likes of the American Optometric Association’s Dr Earl Smith, suggest hyperopic peripheral retinal defocus induces axial length growth and, conversely, myopic peripheral retinal defocus is protective against axial change. This underpins current theory about why multifocal soft contact lenses and ortho-k are useful for controlling myopic growth. Put simply, the relatively steep/increased plus portions within the pupil zone contribute to peripheral myopic defocus, while still focusing light accurately at the fovea. Don’t be taken in by online scaremongers, like endmyopia.org, for most levels of myopia, undercorrection of myopia will increase myopic progression more than an accurate correction³.
The main CL options
The two main soft, multifocal contact lens (SMFCL) designs used for myopia control in this part of the world are both from Coopervision, which is making a real push to dominate the specialty contact lens market worldwide, acquiring the Dutch rigid lens company, Procornea, and well-known ortho-k lens manufacturer, Paragon, last year.
Coopervision’s monthly Biofinity Proclear D multifocal and it’s daily MiSight myopia-control lens (originally designed at the University of Auckland) are both designs that employ a central distance zone and peripheral plus, in different forms.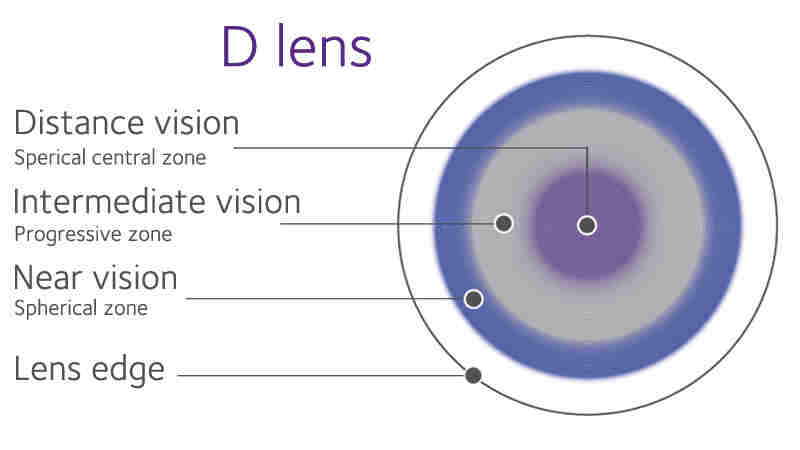
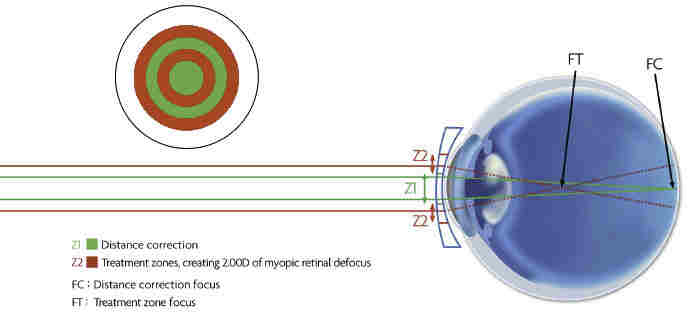
Fig 1 and Fig 2. The Coopervision D lens with its central distance zone and the MiSight lens with its two annuli of +2.00 ‘add’ power
The Proclear D multifocal with a +2.00 add was shown to slow refractive progression by 50% and axial change by 29% over two years in 8-11 year old children⁴. The MiSight three-year results released recently, showed the design reduced myopia progression by 59% refractively and 52% axially compared to a single vision lens control. Another lens, the Acuvue Bifocal, is now no longer on the market. This centre-distance design used similar concentric plus annulus to the MiSight lens and, in a 2016 study, showed a 72% reduction in refractive error progression and 80% reduction in axial elongation⁵.
It is worthwhile addressing the fact that all the lenses touted as myopia control devices are centre-distance designs. So, will a centre-near design also work for myopia control? Due to ortho-k historically being the ‘darling’ of contact lens-based myopia control, there is a school-of-thought to simply mimic the same centre-distance optics created by ortho-k, just on the front surface of a day-wear soft lens. Intuitively this makes sense if we apply the theory of the myopic retinal image shell. With a centre-distance optic, we maintain accurate foveal focus, allow acceptable subjective distance vision and present a myopic defocus in the peripheral retina as off-axis light rays passing through the plus periphery of the lens. However, in myopia control circles there is still no consensus on whether centre-near design may still be effective for myopia control. Several practitioners around the world have shared their experiences from their clinics and found that as long as extra plus is in the system somewhere, a degree of myopia control will be achieved. This may point to different mechanisms of why multifocals affect eye growth. More research is definitely needed!
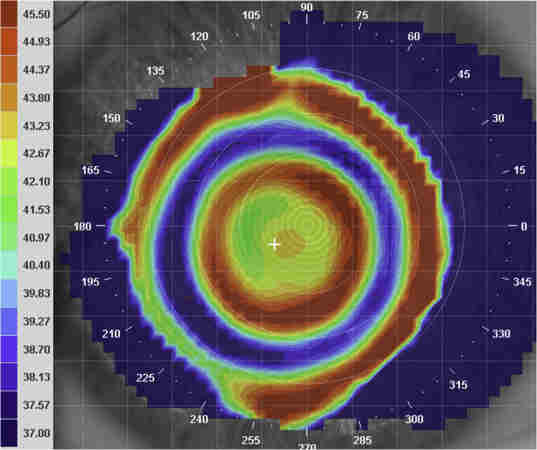
Fig 3. An over-topography of a MiSight contact lens showing the two rings of plus power in the lens design
Pros and cons of myopia control SMFCLs?
The main advantage to practitioners of SMFCLs is the ease of fitting. If you have a slit-lamp you can offer proven myopia control to your patients. From a patient perspective, we know kids love wearing contact lenses and, in my experience, they tolerate the multifocal optics fine. Personally, I prefer fitting daily lenses to children and teenagers, due to the hygiene and convenience aspect. It also makes more sense to the public to use a lens designed and marketed for myopia control, rather than adapting a monthly lens designed for presbyopia in adults.
There is also an argument that SMFCLs may be more effective than conventional ortho-k lenses for levels of myopia below 2D. This has to do with the challenge of creating a significant ring of plus power when the refractive target for the ortho-K lens is only small. In contrast, a MiSight lens has an ‘add’ of +2.00D regardless of whether it is correcting -0.50D or -5.00D of refractive error.
The set ‘add’ of the current soft multifocals, however, are also a weakness in my mind, especially for higher levels of myopia. The beauty of ortho-k is that the higher the correction, the higher the effective ‘add’ in the mid-periphery. It makes sense that the more peripheral myopic defocus, the more myopia control effect possible. A soft lens only providing 2D of peripheral myopic retinal defocus relative to the fovea, may not be sufficient for an already highly-elongated eye. The MiSight studies published only included children with less than -4.00 of myopia. I would be interested to see results from a cohort with higher levels of myopia where, I predict, a lower level of myopia control would be achieved. Anecdotally, patients of myself and colleagues using ortho-k for higher levels of myopia have, in many cases, shown complete halting of their myopia with ortho-k potentially due to the higher levels of peripheral plus created.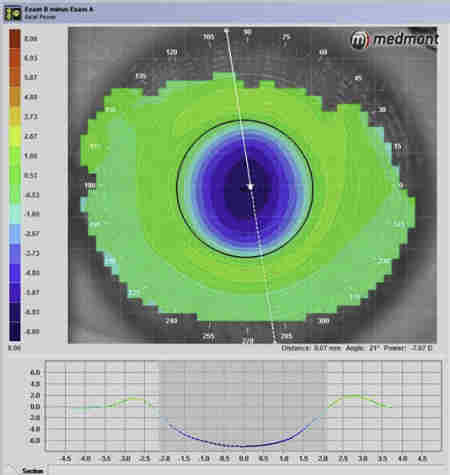
Fig 4. An axial difference map of a -7D ortho-k patient of mine, showing ~9D of plus in the mid-periphery compared to the pupil centre, representing ~4x the ‘add’ possible with a MiSight lens
Also, don’t forget that apart from the rarely prescribed Proclear Toric Multifocal, SMFCLs do not correct for astigmatism which limits their use for myopic astigmats. Ortho-k is generally a better option here as toric corneae can now be effectively moulded and astigmatism corrected using non-rotationally symmetrical ortho-k lens designs.
Alternative SMFCLs on the horizon
New SMFCL designs yet to hit our shores offer some exciting options for our myopia control patients. One in particular, the NaturalVue daily multifocal from Visioneering Technologies, should address my issue with the limited add-levels currently available. This centre-distance lens (made from the same material as the Acuvue 1-Day Moist) is rather unique. The peripheral plus power smoothly, but rapidly, builds up from the centre of the lens to reach a whopping ~20D of relative plus at the edge of the optic zone. This is termed ‘extended depth of focus’. As a multifocal for presbyopes this ‘pinhole’ effect negates the need for different add levels and it seems, in principle, perfect for myopia control applications. The lens is already available in the USA and several retrospective multi-centre studies have been released showing more than 90% reduction in myopia progression with the NaturalVue lens compared to previous treatments⁶.
Oddly, topography over the NaturalVue lens in-situ fails to show the degree of steepening expected. The VTI consultants tell me this is because the degree of plus is so extreme the topographers’ algorithms cannot display the data accurately and instead display the curvature as zones. Interestingly, a similar centre-distance multifocal from ArtMost Oceania, the SoftOK, which is designed to simulate an ortho-k treatment zone, shows the rapid increase in plus in the periphery fine!
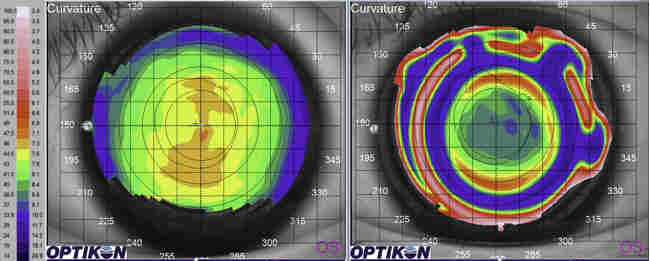
Fig 5. Over-topography of NaturalVue. Note the difficulties the topographer has showing the rapid increase in peripheral plus. Photo courtesy of David Sweeney, supplied by Sally Dillehay, CMO of Visioneering Technologies
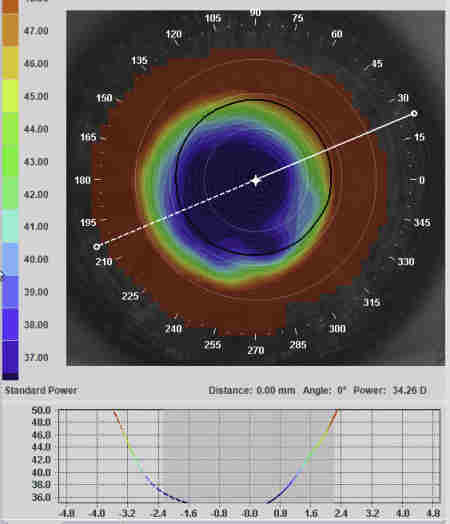
Fig 6. In contrast to Fig 5, the over-topography of the Artmost SoftOK lens clearly shows a steepening periphery not unlike that of a high myopia ortho-k result. Photo courtesy of Paul Levine
Let’s not forget day-wear rigid lens options too! Rigid lens materials offer great physiology for the underlying ocular surface, will correct for astigmatism more effectively than soft designs and are generally more customisable. One example is the hybrid (rigid centre, soft SiHy skirt) Duette multifocal lens from Synergeyes, which was recently made available in a centre-distance option to keep us myopia controllers happy. This lens has customised distance portion optic zone sizes from 1.8-4.0mm and an add range up to +4.00D.
Putting it into practice
I had an interesting and challenging case referred to my clinic at the end of last year. A 10-year-old girl, who was already R -11.00/-1.00x15 (6/5), L -11.25/-1.25x15 (6/5), with axial lengths in the 28mm range. This poor girl had progressed -1.50D in the last year while wearing single vision daily contacts that were now out of range. I posted the case on several online myopia control forums and received a dizzying array of different recommendations for management - soft multifocals, customised soft torics, ortho-k with potential top-up spectacles, the Duette CD multifocal, leaving her in spectacles and single vision contact lenses (on the assumption this level of young myopia was a different clinical entity to ‘normal’ adolescent myopia) and customised RGP multifocals. This was an interesting exercise in itself to see how different practitioners around the world would tackle a tricky case, and highlighted there is no accepted myopia control strategy for every patient.
In the end, because her prescription was too high for me to be comfortable with ortho-k, and her astigmatism ruled out soft mulitfocals, I opted for a dual approach to try and limit future axial progression: atropine 0.02% drops in the evening, combined with a customised myopia control rigid corneal lens. With the help of the Corneal Lens Corporation, the customised lens was designed as a standard bitoric RGP with a 10.5mm diameter for stability. The lens had only a 4mm front optic zone, while outside this was a ring of +3D relative plus for myopia control. The patient could see 6/5 through the lenses and, aside from the normal adjustment required for rigid lenses, is now able to wear the lens comfortably throughout the day. It is too early to say how stable her myopia will be with this combination, but I’ve got my fingers and eyes crossed for this young patient!
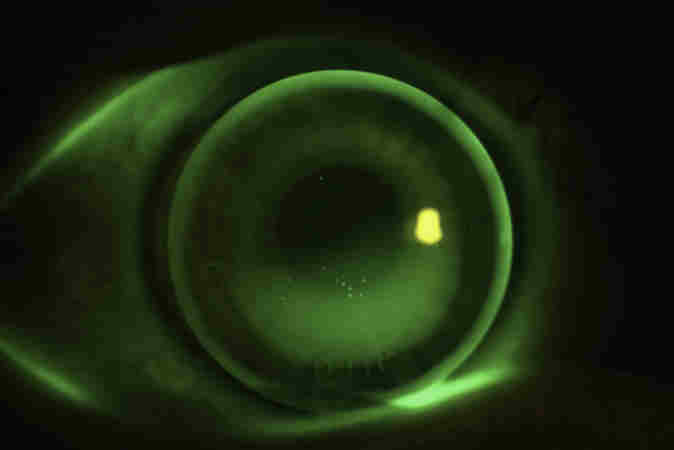
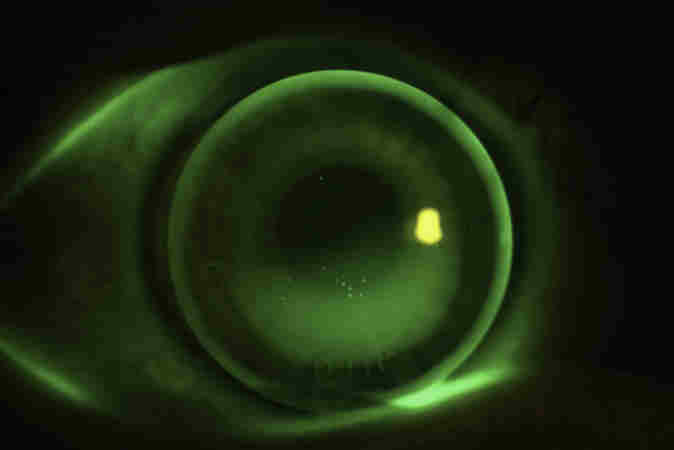
Fig 7. The 10.5mm bitoric rigid corneal lens with myopia control optics fitted to my 10-year-old patient
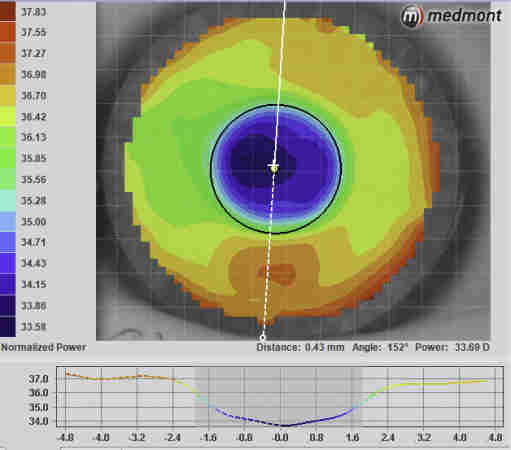
Fig 8. The over-topography of the RGP lens in Fig 6, showing the +3D of peripheral plus outside the 4mm front optic zone
A concluding plea
Around the world, myopia control is starting to be viewed as a standard of care and I implore you not to be myopic when it comes to myopia management (pardon the pun)!
Hopefully this article demonstrates that you don’t have to be an ortho-k guru to make a difference to our young myopes’ lives. Contact lens treatments for myopia control are straightforward and are backed-up by evidence. If you are serious about myopia control, invest in a topographer and begin the journey to learn about ortho-k fitting. It is exciting. Or, at the very least, contact Coopervision to ask how you can start fitting Biofinity MF or MiSight for your patients, and keep an eye out for the new multifocals heading in our direction soon, I hope!
About the author
Alex Petty (BOptom hons, FIAO) is a New Zealand optometrist based at Bay Eye Care in Tauranga, with a particular interest, knowledge and passion for specialty contact lenses, ortho-k and myopia control.
References
- Bullimore MA, Berntsen DA. Low-Dose Atropine for Myopia Control: Considering All the Data. JAMA Ophthalmol 2018;136(3):303
- Gong Q, Janowski M, Luo M, et al. Efficacy and Adverse Effects of Atropine in Childhood Myopia: A Meta-analysis. JAMA Ophthalmol 2017;135(6):624-30
- Chung, Mohindin. Undercorrection of myopia enhances rather than inhibits myopia progression Vision Res 42, 2555-9 (2002)
- Walline et al 2013 Mulitfocal contact lens myopia control. Optometry and Vision Science 90 (11). 1207-1214
- Aller et al 2016, Myopia control with bifocal contact lenses: A Randomised Clinical Trial. Optometry and Vision Science. 93 (4), 344-352.
- Cooper et al. Case Series Analysis of Myopic Progression Control With a Unique Extended Depth of Focus Multifocal Contact Lens. Eye Contact Lens 2017