Optic disc drusen and pseudo-papilloedema
It is a common scenario that potentially swollen optic discs are detected on routine eye examination for another purpose. Clearly, if someone presents with headaches and visual disturbance, then any potentially swollen discs need urgent assessment because papilloedema can be due to life-threatening intracranial problems, such as tumours or vein occlusions. However, it is much more common that people present with presbyopia or dry eye symptoms and the optic disc examination is incidental. In this setting, it is important that the optic discs are examined carefully because true papilloedema can still present without symptoms. Thus, the term pseudo-papilloedema should be used with care.
Causes of pseudo-papilloedema
A clear diagnosis should be sought:
- Myopia with tilted discs may have an indistinct nasal margin
- Hypermetropia with small crowded discs may have no cup, indistinct margins and a thick nerve fibre layer
- Myelinated nerve fibres are obvious white localised opacities in the nerve fibre layer
- Optic disc drusen (ODD) are the most typical cause for a potentially swollen disc without symptoms
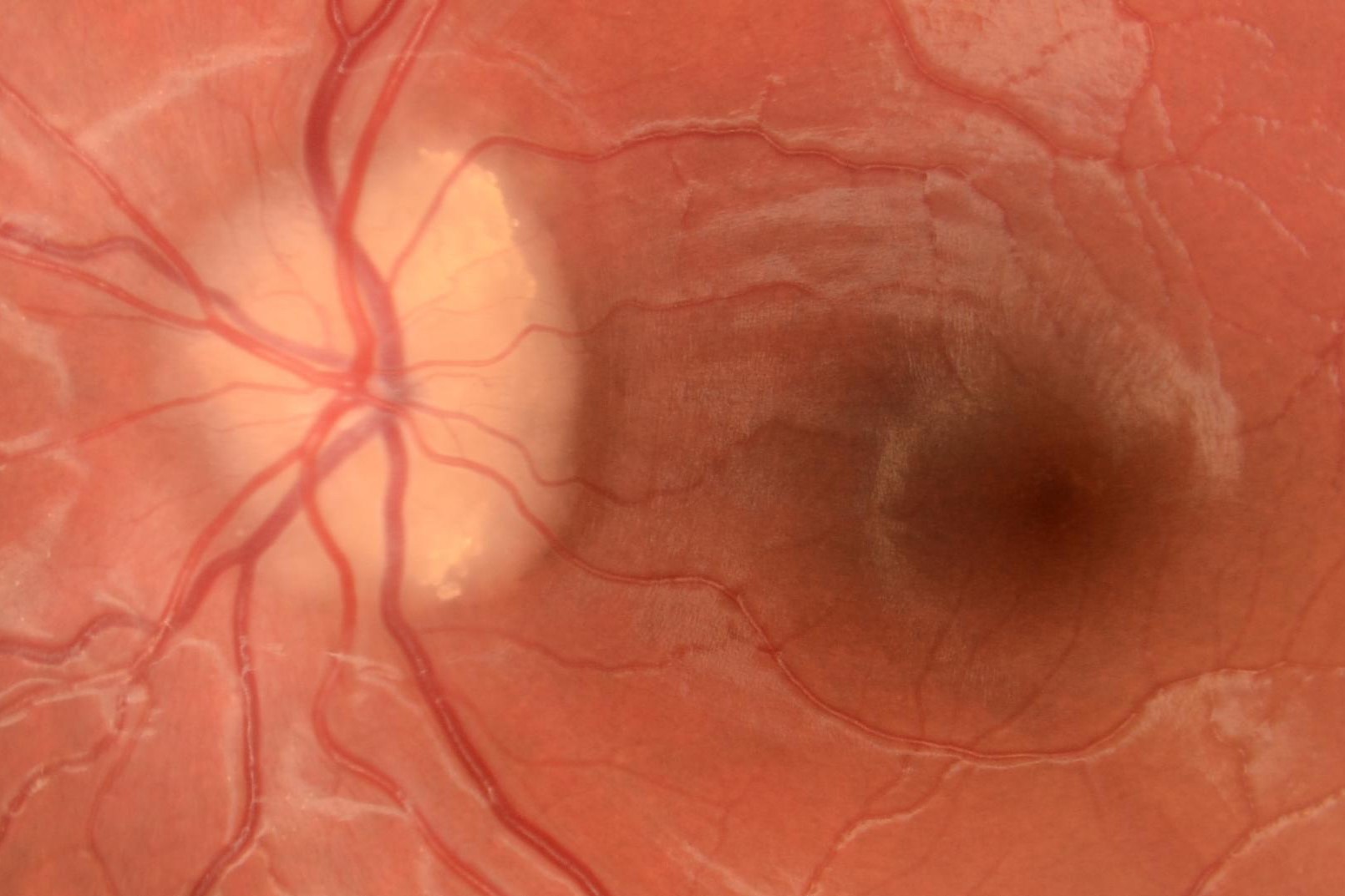
Assuming the patient has no symptoms and normal visual function, it can still be difficult to tell the difference between mild disc oedema and one of these diagnoses. If there are haemorrhages, hyperaemia, microvascular abnormalities, concentric chorioretinal wrinkles (Paton lines), abnormalities of the retina such as cotton wool spots, uveitis, exudates or if the nerve fibre layer is thickened enough to obscure retinal blood vessels at the disc margin, these are all strong indications that this is true optic disc oedema. Even if drusen are visible, there can be concern that the extent of swelling exceeds the amount of drusen (for example obscuring blood vessels, or in presence of a disc haemorrhage) (Figure 1).
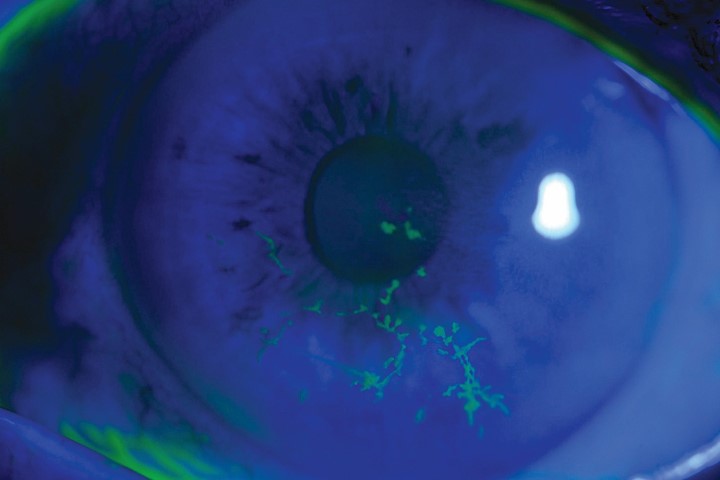
When the diagnosis remains uncertain, two papers from Los Angeles make a good case for using fluorescein angiography to detect true disc oedema with or without ODD¹⁻². When disc drusen are visible there may be pre-injection auto-fluorescence, followed by early nodular staining without leakage. With buried ODD, only 12% were autofluorescent, 25% had early nodular staining, 80% had late circumferential peripapillary staining and none showed leakage. In true disc swelling late leakage is present. Comparing imaging modalities in children or adults, FA appeared to be more sensitive and more specific than other imaging (although there were methodologic problems with these studies)¹⁻². Fluorescein findings remain subjective and there are no firm criteria published. It is also an invasive test and these are the main criticisms which result in not everyone using FA in this context.
To summarise, if patients have symptoms of intracranial hypertension (headache etc.) or reduced vision with swollen discs, they need investigation. If they show haemorrhage, hyperaemia or retinopathy or obscured blood vessels, then they have true disc swelling, which requires investigation. If they have no symptoms or visual loss, and the disc appearance is indeterminate or has potential ODD that do not seem adequate to explain the swelling, then FA can be useful to exclude genuine disc oedema.
Diagnosing optic disc drusen
The preponderance of pseudo-papilloedema is due to ODD. These drusen are benign concretions of acellular calcified glycoproteins that form in the prelaminar optic nerve head (anterior to lamina cribrosa) early in life. They are more common in people who identify as European. Most ODD are asymptomatic, detected incidentally on eye examination (diagnosed prevalence around 0.5%, autopsy prevalence around 2%). When drusen are visible in the superficial layers of the optic disc, they are usually a straightforward clinical diagnosis, but when buried deeper in the disc, they can be difficult to differentiate from optic disc oedema. Buried ODD may have a lumpy appearance, anomalous vascular branching and the nerve fibre layer does not usually have a greyish thickening that obscures blood vessels. Generally, we rely on imaging of some type to confirm the presence of disc drusen and allow us to reassure the patient.
Ultrasonography is sensitive to the presence of calcified drusen of a certain size, generating a bright echogenic focus at the optic disc, even at low gain. False positives can occur, and false negatives are presumed to be from very small drusen.
Computed tomography (CT) will show calcified drusen, but is less sensitive than ultrasound due to thicker slices, and the radiation exposure limits the usefulness of CT.
Magnetic resonance imaging (MRI) is now indispensable in cases of disc oedema but has no ability to detect ODD.
Autofluorescence imaging can be obtained with a retinal camera and fluorescein filters, but more sensitive detection is obtained with scanning laser ophthalmoscopy, eg. in Spectralis optical coherence tomography (OCT). Visible ODD produce bright hyper-fluorescent foci in the disc (understood to be calcium salts). Buried drusen give a reduced fluorescence related to the thickness of overlying tissue and, in these buried ODD, autofluorescence had approximately half the sensitivity of ultrasound.
Both enhanced depth imaging (EDI) and swept source OCT have improved the penetration and resolution of deeper tissues in the disc. These two technologies appear more sensitive in detecting drusen than standard spectral domain OCT. A hyper-reflective bulge in the subretinal space adjacent to the disc margin is not ODD and can occur in papilloedema. Rather, ODD are seen as irregular hypo-reflective structures, with hyper-reflective foci or bands in the surface of the ONHD. Similar hyper-reflective bands without a hypo-reflective core may indicate small drusen, although this has not been corroborated³⁻⁴. Studies have shown that in suspected buried drusen, EDI OCT is the most sensitive and standard OCT is more sensitive than ultrasound³. It is not yet clear how to use the OCT to differentiate true disc oedema from ODD; the retinal nerve fibre layer (RNFL) can be increased or decreased in thickness in both drusen and in papilloedema⁵.
Prognosis and progression
The prognosis for ODD is favourable and most patients are reassured and discharged. A range of visual field defects are common, particularly with visible ODD, and these correlate with RNFL defects. Fields may deteriorate slowly over time, probably at a faster rate than normal eyes⁶. In this way, ODD may resemble glaucoma. Some well-documented cases with long follow-up indicate that ODD can become more visible with worsening of visual field in the first few decades of life, but then remain fairly stable in adulthood⁷⁻⁸.
When visual fields slowly deteriorate in adulthood, there is often uncertainty about treating ODD as a type of glaucoma. Because the disc appearance is atypical, glaucoma is usually diagnosed in the presence of raised intraocular pressure (IOP) and progressive field loss. In one cross-sectional study, ODD eyes with raised IOP had more visible drusen and more field defects than ODD eyes with normal IOP⁹, but another cohort found no association between IOP and field defect or nerve fibre thickness in patients with ODD¹⁰.
Disc drusen complications
Disc drusen appear to be a risk factor for non-arteritic anterior ischaemic optic neuropathy (NAION), although this has been hard to quantify and confirm. The presentation of NAION with ODD is sudden painless vision loss, with increased disc swelling and haemorrhages. The presence of ODD should not distract from the investigation of an acute optic neuropathy. Occlusions of central retinal vein or central retinal artery have also been reported in eyes with ODD in occasional cases. Peri-papillary choroidal neovascular membranes (CNV) are common, benign, and often asymptomatic in eyes with ODD, but progression under the macula may affect acuity and warrant treatment. Small peri-papillary haemorrhages at different layers, without any clinical evidence of CNV, are also common and benign.
Conclusions
Potentially swollen optic discs can be stressful as they could represent the first sign of life-threatening pathology. As always, a history and examination can clarify most cases, and our increasing array of investigations can sort out the rest. Much remains unknown about ODD, particularly the crucial factors that affect progressive field loss in adulthood. New electrophysiology techniques to measure stress on retinal ganglion cells may shed light on how drusen deteriorate over time and allow more rapid testing of treatments.
References
- Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. J Neuroophthalmol. 2012;32(1):17-22.
- Chang MY, Federico GV, Demer JL, Bonelli L, Quiros PA, Arnold AC, Sadun AA, Pineles SL. Accuracy of Diagnostic Imaging Modalities for Classifying Pediatric Eyes as Papilledema Versus Pseudopapilledema. Ophthalmology. 2017;124:1839-48.
- Merchant KY, Su D, Park SC, Qayum S, Banik R, Liebmann JM, Ritch R. Enhanced depth imaging optical coherence tomography of optic nerve head drusen. Ophthalmology. 2013;120(7):1409-14.
- Malmqvist L, Bursztyn L, Costello F, Digre K, Fraser JA, Fraser C, Katz B, Lawlor M, Petzold A, Sibony P, Warner J, Wegener M, Wong S, Hamann S. The Optic Disc Drusen Studies Consortium Recommendations for Diagnosis of Optic Disc Drusen Using Optical Coherence Tomography. J Neuroophthalmol. 2017.
- Palmer E, Gale J, Crowston JG, Wells AP. Optic Nerve Head Drusen: An Update. Neuroophthalmology. 2018;42(6):367-84.
- Lee AG, Zimmerman MB. The rate of visual field loss in optic nerve head drusen. Am J Ophthalmol. 2005;139(6):1062-6.
- Malmqvist L, Hamann S. Photographic Documentation of Optic Disc Drusen Over More Than 50 Years. JAMA ophthalmology. 2017;135(3):e165470.
- Spencer TS, Katz BJ, Weber SW, Digre KB. Progression from anomalous optic discs to visible optic disc drusen. J Neuroophthalmol. 2004;24(4):297-8.
- Grippo TM, Shihadeh WA, Schargus M, Gramer E, Tello C, Liebmann JM, Ritch R. Optic nerve head drusen and visual field loss in normotensive and hypertensive eyes. J Glaucoma. 2008;17(2):100-4.
- Nolan KW, Lee MS, Jalalizadeh RA, Firl KC, Van Stavern GP, McClelland CM. Optic Nerve Head Drusen: The Relationship Between Intraocular Pressure and Optic Nerve Structure and Function. J Neuroophthalmol. 2017.
Dr Jesse Gale is a consultant ophthalmologist at Capital & Coast District Health Board and Capital Eye Specialists, and a senior clinical lecturer at University of Otago, Wellington. He has subspecialty interests in glaucoma and neuro-ophthalmology, and current projects include open-source devices, electrophysiology, and a national data network.