Refractive surgery evidence review
Dissatisfaction after implantation of EDOF intraocular lenses
Wanten J, Bauer N, Berendschot T, van der Biggelaar F, Nuijts R J
Cataract Refract Surg 2025; 51: 399-405
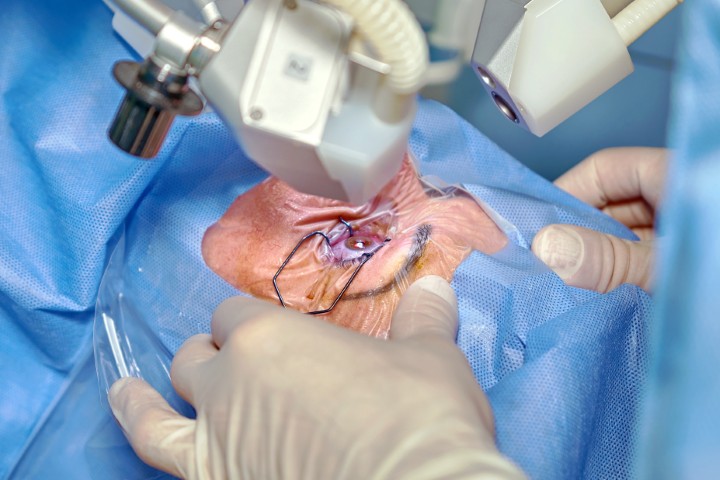
Review: In this retrospective case review the authors explore the causes of dissatisfaction following implantation of extended-depth-of-focus (EDOF) intraocular lenses (IOLs). The study is based on a real-world experience with the Acrysof IQ Vivity IOL. A low threshold for dissatisfaction was applied, where a patient reporting even a minor level of concern met criteria for inclusion.
Of the 354 eyes which underwent EDOF IOL implantation, 82 (22.8%) patients reported any level of dissatisfaction. Blurred vision (94%) and photopic phenomena (25.3%), with coexistence in some cases, were the predominant patient-reported complaints. The main causes were residual ametropia (51.8%), dry eye disease (26.5%) and posterior capsular opacification (12%). Following additional treatment, most patients achieved satisfaction (85.5% of those initially dissatisfied) resulting in 5.9% of the entire patient cohort remaining dissatisfied.
Comment: An important topic to highlight from this paper is the impact of residual ametropia on EDOF IOLs. Previously, EDOF IOLs have been thought to exhibit greater tolerance for residual ametropia, especially with regard to astigmatism. The authors of this study aimed to target residual postoperative refractive astigmatism of 1D or less. However, their findings in the context of achieving patient satisfaction were that the level of tolerance was between 0.50–0.75D, comparative to trifocal optics. Overall, 12.9% of patients required refractive laser enhancement to achieve their desired refractive outcome. Refractive targets for EDOF IOLs, including astigmatism correction, should be treated with the same level of precision as trifocal optics.
Myopic regression after FS-LASIK and SMILE
Lin Meng-Yin, Tan Hsin-Yuan, Chang C
Cornea; 43:1560-1566
Review: A propensity score method was used to retrospectively match patients who had undergone femtosecond laser in-situ keratomileusis (FS-LASIK) or small-incision lenticule extraction (SMILE) laser vision correction for myopia. Myopic regression was defined as a myopic shift of greater than 0.50D compared with the one-month postoperative spherical equivalent refraction (SEQ).
Comment: There was no significant difference in myopic regression following FS-LASIK or SMILE procedures. Consistent with other evidence, the strongest correlation with myopic regression was a reduced optical zone (OZ, 6.2mm or less), due to the necessity of reducing the OZ when treating higher levels of myopia to conserve tissue. The authors of this study used OZ zones less than 6.0mm, which is outside of standard practice – this may have been due to the high average SEQ of patients included in the study (-6.77D).
A major limitation of this review was the lack of axial length measurement to ascertain whether the myopic shift was due to corneal remodelling following surgical intervention or progressive axial myopia. The authors used an emmetropic target for all patients aged 21–39 years. Many refractive surgeons would advocate for a low hyperopic target (+0.25-0.50D) in patients under 30 years of age.
Despite similar results in postoperative SEQ, SMILE demonstrated a lower rate of enhancement – 1.3%, compared with 4.9% in the FS-LASIK group. The FS-LASIK group, however, demonstrated a significantly higher residual stromal thickness and reduced ablation depth for the same level of myopic correction.
Evidence-based guidelines for keratorefractive lenticule extraction surgery
Wang Y, Xie L, Yao K, Sekundo W, Alio J et al
Ophthalmology 2025; 132: 397-419
Review: This recently published review provides evidence-based guidelines for keratorefractive lenticule extraction (KLEx), the most common iteration being SMILE. A total of 250,717 studies were assessed, with 609 included in 26 systematic reviews undertaken to generate the guidelines. The guidelines detail 38 recommendations covering three domains: indications, surgical planning and technique, and complications. Each recommendation is graded with regard to evidence quality and strength.
Comment: The guidelines have been developed due to the increasing uptake and variation of KLEx procedures. Many of the recommendations made would be considered standard practice for experienced surgeons utilising the SMILE Pro platform.
Several recommendations note the potential preservation of corneal biomechanical parameters compared with traditional FS-LASIK. KLEx procedures have demonstrated greater preservation of corneal resistance and hysteresis. However, consistent with the paper above, KLEx often results in a lower residual stromal bed for an equivalent SEQ correction, which has historically been considered an important risk factor for postoperative ectasia. While early rates of postoperative corneal ectasia in KLEx (0.02%) suggest a lower incidence than FS-LASIK (0.09%) due to the relatively novel application of KLEx, long-term data are required to ensure this impact is sustained. A conservative residual stromal thickness of at least 280μm and lenticule thickness >28% of central corneal thickness is recommended. Stringent preoperative assessment for risk factors of ectasia remains essential.

Dr Zea Munro is a cataract and refractive surgeon who has recently returned to New Zealand to join the team at Christchurch’s Fendalton Eye Clinic following her international fellowship.