Retina NZ: innovation in retina research
Retina New Zealand’s inaugural Summer Symposium, Australasia 2025, was held over two days in February. The peer-based group supports individuals living with retina-associated vision loss, primarily focusing on inherited retinal diseases (IRDs). As an affiliate of Retina International, one of its core missions is to advance research aimed at treating blindness.
Focused on the theme ‘Innovation in Retina Research’, the symposium’s first day was dedicated to eyecare professionals, while the second welcomed the public, including those with retinal diseases. Attendees explored the latest treatment breakthroughs, including advancements in biomarker research and emerging technologies shaping the future of eye health.
Both days began with three lectures delivered by the keynote speakers, Professors Lauren Ayton and Robyn Guymer from the Centre for Eye Research Australia (CERA) and Dr Lola Mugisho from the University of Auckland.
Head of CERA’s Retinal Gene Therapy Unit and the Vision Optimisation Unit at the University of Melbourne, Prof Ayton updated us about emerging IRD therapies. It was interesting to learn that since the US Food and Drug Administration (FDA) approved Luxturna in 2017 – the first gene therapy for RPE65-associated inherited retinal degeneration – the race has been on for the next breakthrough treatment. Prof Ayton highlighted that despite growing interest, understanding of gene therapy among patients remains limited. In collaboration with the Foundation Fighting Blindness, her research aims to improve global knowledge-sharing to bridge this gap.

Prof Lauren Ayton
She also discussed several promising therapeutics under development, the most fascinating being Nacuity’s NPI-001 (an oral antioxidant to slow vision loss in patients with retinitis pigmentosa and Usher Syndrome), Kiora Pharmaceuticals’ photoswitch therapy KIO-301 (which stimulates retinal ganglion cells to detect light in place of degenerated photoreceptors) and CERA spin-out Mirugen’s retinal stem cell therapy.
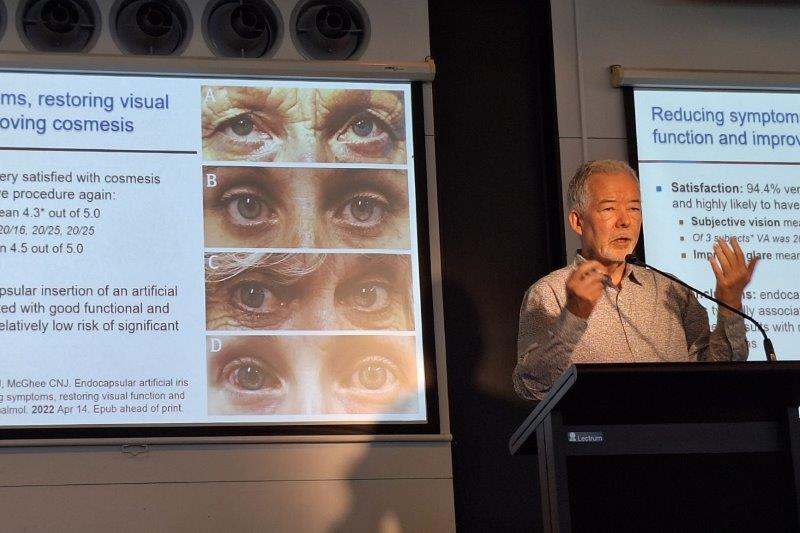
Alternative anti-VEGF avenues
CERA deputy director Prof Guymer’s lecture, ‘Addressing clinical limitations in AMD treatments’, discussed the patient burden of frequent anti-VEGF intravitreal injections and their diminishing efficacy over time. Despite their well-documented effectiveness at halting leakage and stabilising vision, real-world studies from her research group showed that only 12% of patients retain driving visual acuity and 15% retain reading visual acuity in at least one eye over an average of 11 years – much lower than clinical trial results suggest. This underscores the urgent need for better and longer-acting anti-VEGF drugs, said Prof Guymer. The increased complications associated with anti-VEGF, such as fibrosis and retinal atrophy, also drive the need for more research into alternatives.

Prof Robyn Guymer
Some novel therapies aiming to circumvent these limitations include sozinibercept (OPT-302, Opthea), which inhibits the broader VEGF family by targeting VEGF-C/D in addition to VEGF-A; faricimab (Vabysmo), the first bispecific antibody targeting both VEGF-A and angiopoietin-2, which is necessary for anti-VEGF stability and reducing inflammation to prevent fibrosis and atrophy; and ABBV-RGX-314 and 4D-150, a gene therapy which increases the expression of several proteins known to act as downstream VEGF inhibitors.
Existing anti-VEGF drugs are also being modified in dosage or mode of delivery. For instance, aflibercept 8mg every 12 or 16 weeks has been shown to better preserve vision and provides more effective drying effects than the same drug used 2mg every eight weeks. In another example, the Port Delivery System, a permanent refillable implant in the sclera, could be used to deliver ranibizumab (Lucentis) passively into the vitreous without interruption for up to six months.
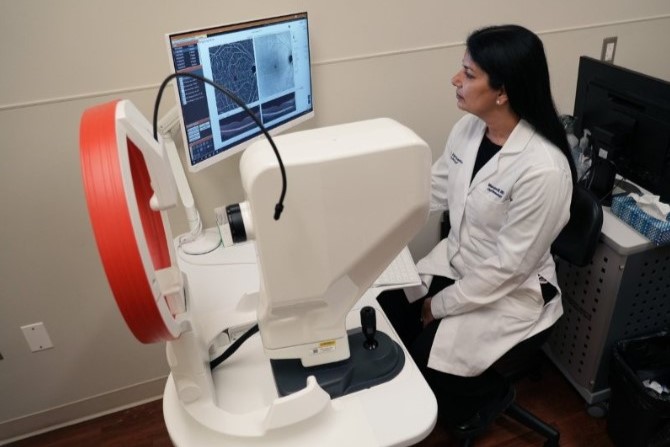
Dr Mugisho, a senior research fellow and deputy director of the Buchanan Ocular Therapeutics Unit and director of the Inflammasome Biology Research Group at Auckland University, presented her team’s research on ‘The role of inflammasome activation in retinal diseases’. Dr Mugisho explained that inflammasomes form part of our innate immune system and usually act as a first line of defence against pathogens. Over the past 10 years, her team has uncovered the significant role they also play in diabetic retinopathy (DR) showing, through preclinical models, that targeting the inflammasome pathway can effectively reduce clinical and molecular signs of DR. Her research also showed inflammasome activation correlates with the transition from diabetes to DR, with C-reactive protein (a biomarker often measured as a part of routine blood tests in clinical practice) reflects inflammasome activation and disease progression. These findings supported the development of tonabersat, an anti-inflammasome drug currently in phase 2b clinical trials for diabetic macular oedema. Her latest research, implicating the inflammasome pathway in IRDs, could therefore pave the way for novel treatment strategies for these diseases.

Dr Lola Mugisho
Cutting-edge Kiwi research
Following the keynote talks were some equally interesting introductions to innovative research from New Zealand. Auckland University’s Dr Jordan Lloyd presented his work on improving our understanding of retinal signalling through voltammetry. Unlike previous studies relying on stained tissue sections or vitreous samples, this technique measures live retinal dopamine. Reduced levels of this key neurotransmitter in retinal function and eye development are linked to Parkinson’s disease and myopia.
Dr Alix Coysh from the University of Auckland’s Applied Translational Genetics Lab shared her work with mentor Professor Russell Snell on establishing large-animal models of RP. With financial support from Retina NZ, she aims to utilise CRISPR/Cas9 genome-editing technology to generate RP models in sheep, paving the way for better understanding of disease progression and preclinical testing of gene therapies.
There were also two interesting talks on emerging technologies for retinal disease prediction and monitoring. Dr Wilson Pan, a research fellow at the Molecular Vision Research Cluster, University of Auckland, highlighted how magnetic resonance imaging can be used to non-invasively measure oxygen tension and viscosity in the vitreous, with both metrics being known to change with disease. His work suggests the vitreous may act as an oxygen sink, protecting the lens from oxidative damage. The absence of vitreous, such as after vitrectomy, could therefore accelerate cataract formation – a hypothesis warranting further investigation. Dr Prakash Karn, an engineer with expertise in artificial intelligence (AI) and machine learning, presented work from his PhD project, which explored innovations in AI for precision diagnosis of retinal diseases. By training AI algorithms on large datasets of retinal images and clinical metadata, his research was able to detect subtle retinal changes as early indicators of systemic diseases.
Dr Francesc March de Ribot, consultant ophthalmologist at Dunedin Hospital, presented his work titled, ‘Vision loss and dementia risk in New Zealand’. Using interRAI software, his team has been analysing correlations between vision loss and dementia in older New Zealanders over the last two years. Their results showed vision loss increased the risk of dementia by 1.55 times and dependence limitations by 1.75 times, with Pasifika populations particularly overrepresented. Interestingly, patients with longstanding vision loss exhibited better cognitive outcomes. Dr March de Ribot posited that individuals who experience vision impairment at an earlier age may have developed compensatory mechanisms, such as belonging to social groups and use of reading aids, which may limit their risk of poor cognitive outcomes as they grow older. Dr Sarah Hull, a senior lecturer at the University of Auckland and an ophthalmologist specialising in paediatrics, genetics and strabismus, presented a case series on recent advances in the understanding of familial exudative vitreoretinopathy and Stickler syndrome, as well as treatment approaches.
The Retinal NZ Summer Symposium 2025 highlighted the rapid evolution of retinal research, from emerging gene therapies to novel anti-inflammatory and AI-driven diagnostic tools. With collaborations between clinicians, researchers and patient organisations, these innovations offer hope for improving visual outcomes and quality of life for people with retinal diseases across Australasia.
Recognising the importance of collaboration between Australasia’s retinal researchers, the Retina NZ symposia series is expected to take place every two years, aiming to drive research forward, share vital information and play a key role in education and scientific progress in New Zealand. Retina New Zealand has a range of publications to help patients and their whānau gain a better understanding of their condition. These, along with recordings of this inaugural symposium, can be requested via admin@retina.org.nz.

Dr Charisse Kuo is a therapeutically qualified optometrist with a PhD in ophthalmology from the University of Auckland. Her research involves the development of tissue-culture models using donor retinas and choroids to explore the mechanisms behind diabetic retinopathy.