Case study: Never judge a book by its cover, or a patient by their visual acuity
Mrs D, an independent 83-year-old who’s very active in church activities and several committees, complained of frustration with her optometrist for not getting her reading prescription right. She loves reading and crosswords but was struggling to do either, see food on her plate, prices and directions on food packets, or menus in restaurants and her papers at committee meetings.
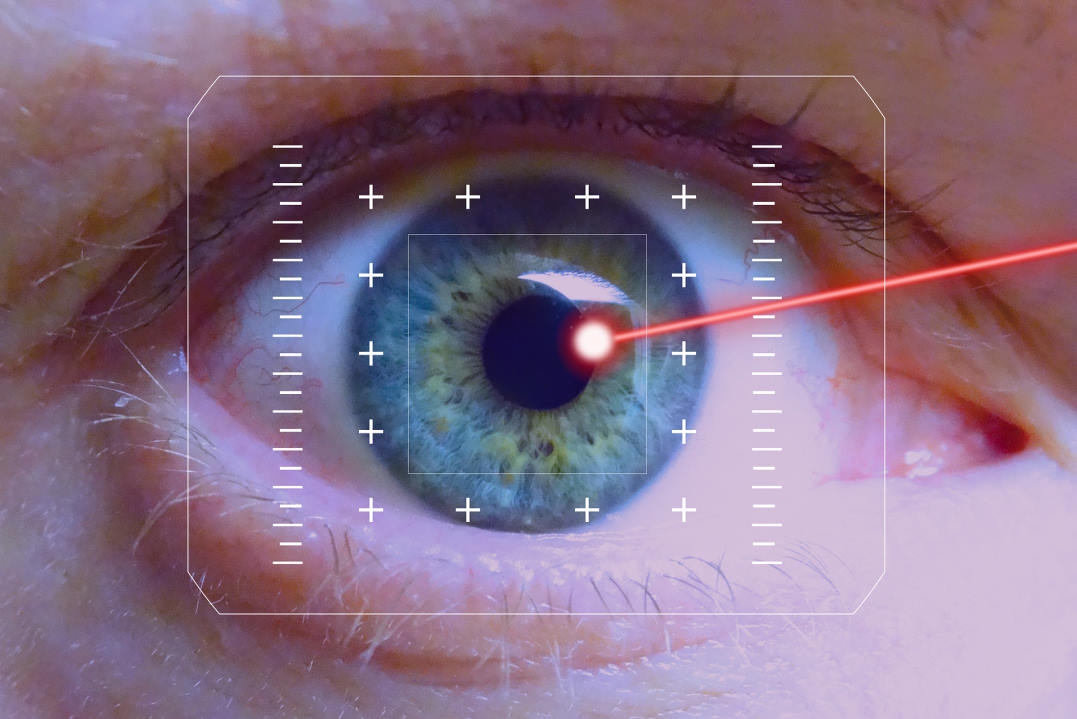
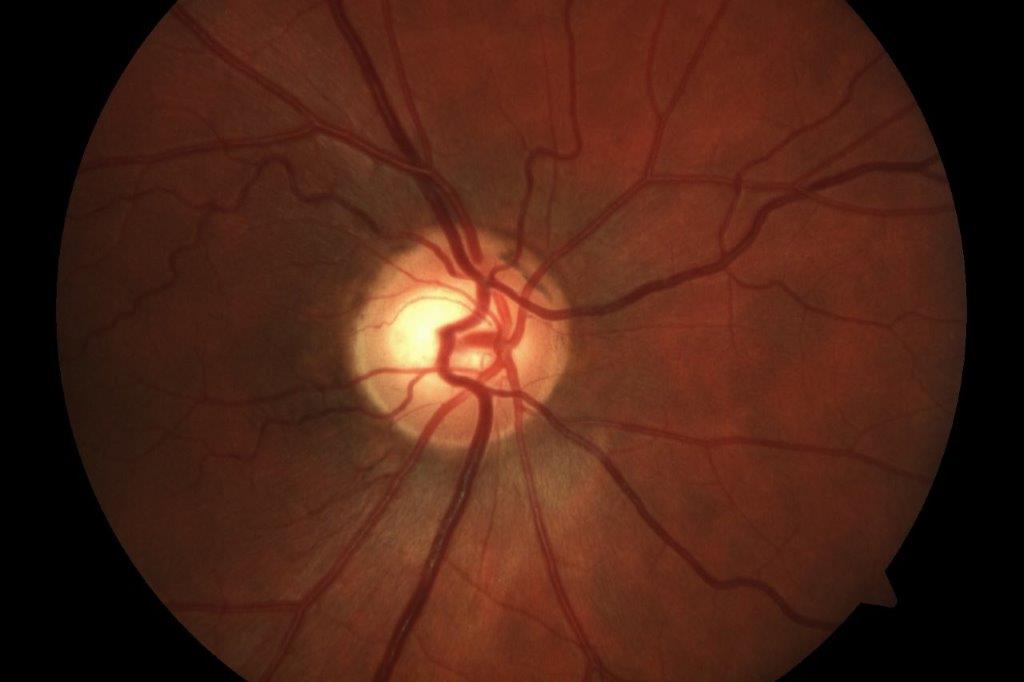
Her ocular history, according to her ophthalmologist’s most recent report, included atrophic macular degeneration in the right eye and several injections of Avastin (bevacizumab) in the left eye for neovascular macular degeneration. She also had a long history of glaucoma, well managed with medication, and is a bilateral pseudophake. Her corrected visual acuity was recorded as RE 6/9, LE 6/15+ binocularly 6/9+, with her latest prescription, according to her optometrist, being RE +1.00-0.75 x 99, add +3.00; LE +0.50-0.50 x 97, add +3.00. Binocular functional visual fields revealed a dense parafoveal ring scotoma with sparing of most of the central 5° (Fig 1).
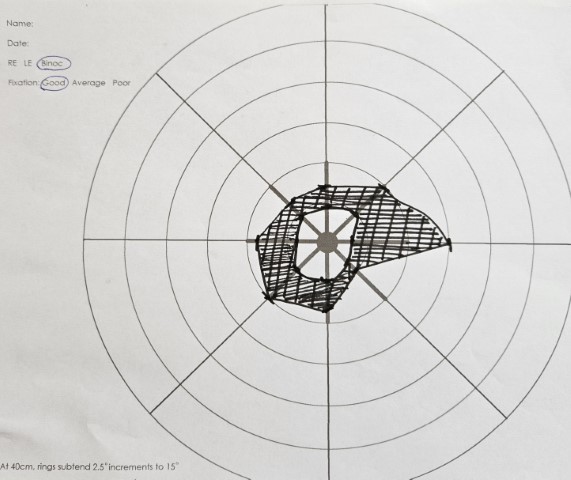
Fig 1. Binocular functional visual fields revealing a dense parafoveal ring scotoma with sparing of most of the central 5 degrees
A ring scotoma always presents a challenge, since, depending on the size and shape of the useable central area, magnification can make reading more difficult as the image is projected into the non-seeing ring, making words patchy with missing or overlapping letters. Small amounts of magnification may allow the maximum use of the remaining central area. Alternatively, higher magnification may be required to project the image beyond the scotoma and onto areas of the retina where the image is degraded, then the words may look patchier. The patient may reject this as it counters the natural instinct to use the better vision in the remaining central area. Use of high magnification also appears contrary to what is indicated by the distance acuity and is therefore often overlooked when seeking a solution.
The issues
Measured on a high-contrast, single-word logMAR reading chart, I recorded Mrs D’s binocular near acuity as N16, improving to N8 when light was applied directly onto the chart. I also noted she had been very hesitantly picking out single letters in the larger words at the top of the chart but gaining confidence and speed as she read down to the smaller lines. This was unsurprising since I knew about the ring scotoma. She improved further to N5 on the continuous text chart, which added meaning to what she was reading. On the low-continuous text chart, her acuity was reduced to N80 single letters, which did not surprise me either, given her history of glaucoma (albeit well managed medically) and macular degeneration.
All this information pointed to a strategy of minimal magnification and maximal enhancement of contrast to achieve fluent and comfortable reading. This requires intense white task lighting or technology that converts low-contrast or coloured print to high-contrast bold black print on white background (or reverse contrast white on a black background if glare from the background is a problem). Various low-vision aids were trialed, with an emphasis on contrast enhancement.
A successful outcome
Mrs D purchased an LED Duo lamp (Fig 2), which has a nice white light on a flexible stand, enabling her to bring the light close for maximum intensity. Using it, she was able to read newsprint comfortably and fluently. She also purchased a rechargeable LED travel lamp (Fig 3) which she can place on her dining table to illuminate the food on her plate or bring to committee meetings to help her read her papers. For extra mobility, to keep in her handbag for use in shops or restaurants, she purchased an Eschenbach 3x magnification LED-illuminated easyPOCKET pocket magnifier (Fig 4).
Fig 2. LED Duo lamp in different configurations
Keeping her reduced contrast sensitivity in mind, it was important to be mindful of glare control. Although Mrs D finds glare a problem, she only wears her sunglasses on the sunniest days as she feels she does not see well with them. A polarized, yellow, non-prescription fitover lens gave her relief from glare and enhanced contrast, and the impression of improved vision. The fitover can also be removed quickly when entering a dark environment.
Fig 3. Portable travel lamp

Fig 4. Eschenbach 3x easyPOCKET magnifier
The final word
Mrs D now has a greater understanding of her problems as well as sufficient assistive aids to help her, provided she retains that little island of central vision. In my report to her ophthalmologist, with a copy to her optometrist, I pointed out Mrs D has a birthday coming up and will be wanting to renew her driver’s licence!

Naomi Meltzer is an experienced optometrist who now runs an independent practice in Auckland specialising in low-vision consultancy. She is a regular contributor to NZ Optics.