Dry eye management at a level that works for you!
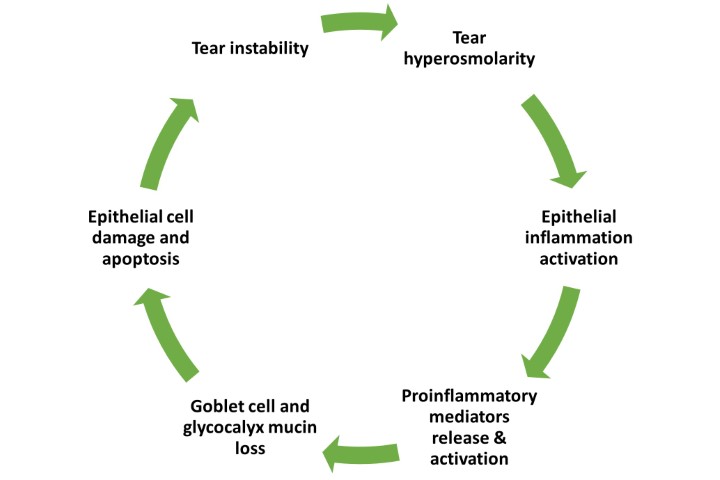
In the six years since publication of the evidence-based TFOS DEWS II reports¹, awareness and acknowledgement of dry eye disease (DED) as a growing global concern has continued to intensify. These reports reached consensus with respect to the diagnosis, classification, diagnosis and management of DED while helping guide better understanding of its epidemiology and pathophysiology, and more eye care practitioners (ECPs) than ever are choosing to rise to the challenge of helping patients address dry eye problems.
In 2022, recognising the importance of making dry eye management widely accessible, the World Council of Optometry saw a need to reassure and encourage ECPs who might be cautious about getting involved due to a perceived lack of resources. Thus it embarked upon a mission, in partnership with Alcon and with the assistance of three TFOS DEWS II subcommittee chairs, Professor James Wolffsohn, Professor Lyndon Jones and me, to show just how easily all practitioners can help a great majority of patients with dry eye disease. The resulting Dry Eye Wheel was developed as an easy-to-use clinical tool that helps direct DED mitigation, measurement and management, even where resources are limited, whether that be in terms of equipment, specialist knowledge or time available to spend with patients.
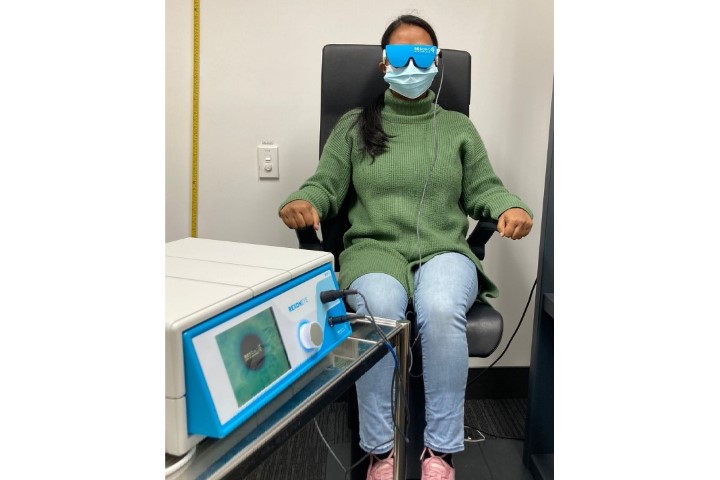
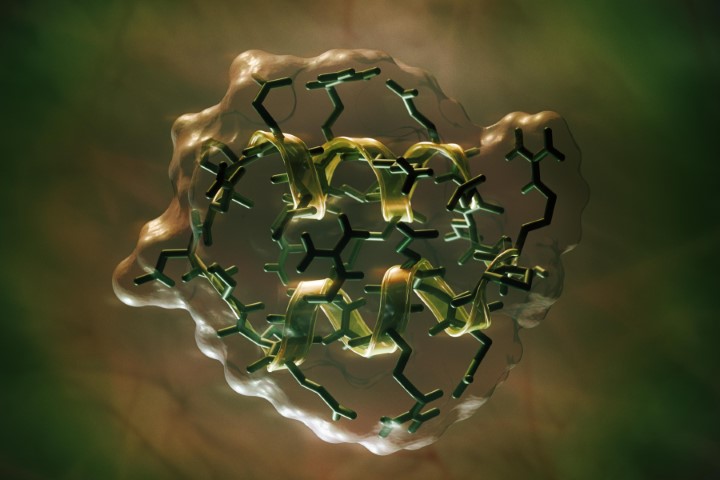
The wheel is divided into three interlocking sectors – mitigation, measurement and management – and offers three levels of complexity, depicted as bronze, silver and gold rings. The largest outer ring, bronze, reflects the largest proportion of the dry eye community who might be identified with simple testing as having mild-to-moderate dry eye; the management section indicates that such patients can often be managed with careful advice and simple, relatively inexpensive, patient-applied treatment strategies.
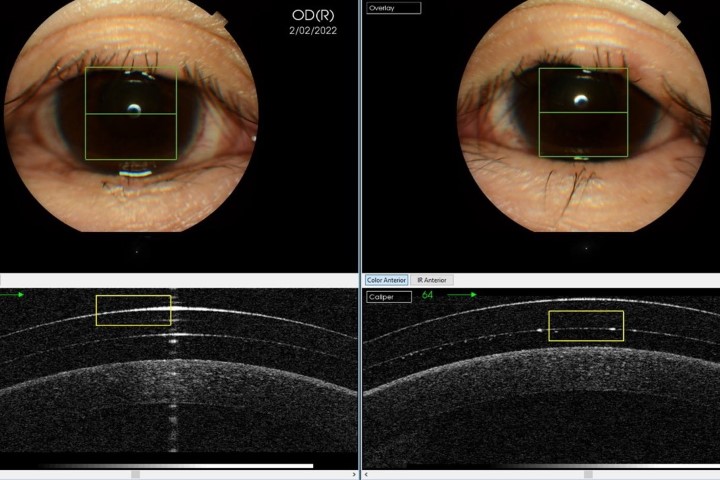
ECPs interested in investing a little extra to upskill their knowledge, devote more chair time and/or invest in equipment will easily find themselves transitioning to the silver zone, allowing them to offer care to an even wider range of patients, including some trickier cases.
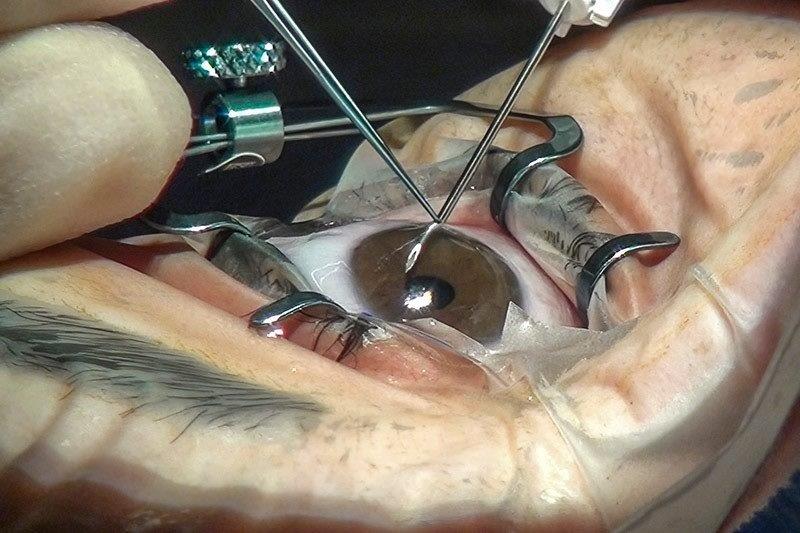
The most complex cases, which may demand more advanced knowledge and/or require management using more costly or technically advanced equipment, are represented in the smallest gold zone, reflecting the relatively small proportion of dry eye patients to whom this would apply and for which they may require referral to a colleague. Care in this case is typically restricted to ECPs and practices with a more specialist interest in DED and a commitment to investment in time and costs.
A series of free webinars describing development and application of the Dry Eye Wheel and an interactive version of the Dry Eye Wheel can be accessed via the World Council of Optometry’s website.
Reference
1. Craig J, Nelson J, Azar D, Belmonte C, Bron A, Chauhan S, et al. TFOS DEWS II Report Executive Summary. Ocul Surf. 2017;15(4):802-12.

Professor Jennifer Craig heads the Ocular Surface Laboratory in the Department of Ophthalmology at the University of Auckland. She is the TFOS ambassador for New Zealand and a member of the TFOS board and was chair of the TFOS Lifestyle Workshop and vice chair of TFOS DEWSII.