Insights and eye-openers from EI's 30th
One would think that after its 29th annual conference, there wouldn’t be much left to talk about, but the Eye Institute (EI) managed to come up with another relevant and interesting programme for its 30th event.
After a breakfast filled with guilty pleasures, Dr Will Cunningham brought the mood down to earth with the serious topic of the growing crisis of diabetic eye disease in the Pacific. He presented a documentary made by one of his diabetic patients, focusing on a tsunami of multigenerational diabetes across the Pacific, with Nauru leading the wave with 34.4% of the population having diabetes, followed by Samoa (27.2%), Tonga (19.6%), Fiji (17.7%) and New Zealand (6.6%), with Polynesians over 65 making up 50% of that Kiwi figure. Overall, one in four is now living with diabetes.
Nauru suffers the ignominious title of being the most obese nation in the world. Once upon a time, diabetes did not exist (or was extremely rare) in the Pacific, he said, so what is causing the tsunami – is it a post-Westernisation lifestyle disease?
With diabetes, high blood sugar leads to endothelial changes in the small blood vessels. The vessels bulge, leak fluid and bleed, which goes on to cause ischaemia. Whatever is happening in the eye is also happening elsewhere in the body – and ischaemia is bad wherever it occurs.

Germaine Joblin and Dr Will Cunningham
Dr Cunningham is on the board of the Fred Hollows Foundation (NZ) and has a personal interest in this subject, revealing that his Samoan grandmother died of diabetes. The work of the Fred Hollows Foundation is prevention of blindness in the Pacific. Its strategy for the Pacific includes support for healthcare strengthening, workforce development and a shift to a sustainable locally led model.
As diabetes is a multigenerational issue, Dr Cunningham encouraged us to tackle it through educating parents and children, not by lecturing them but by connecting with them. “The hook,” he said, “is the family. Relate it to the family: ‘This is what it is going to look like for your family if you don’t take control of this early enough’.”
Practise before practice
Dr Adam Watson’s topic of the practical ethics of using AI scribes in practice started with a nod to the difficulty of finding that elusive single ethics point to complete the optometrists’ biannual CPD points cycle. There were several references throughout the day to the stress this causes many optometrists, as the renewal of registration depends on finding this and its partner – the single point on cultural safety – by the deadline.
Scribes have traditionally been used in secondary and tertiary education, when a student is unable to write the answers themselves, or in law courts where a recording device may not be reliable. What is the role of an AI scribe in eyecare? Generative AI uses speech recognition software to take the information it is recording and distills it into what is useful. This, according to Dr Watson, affords better quality communication with the patient because the practitioner is not thinking about note taking or employing extra staff to do so, costing money and introducing another person to the room, which the patient may not be entirely comfortable with.
I’d agree with Dr Watson on this. For me, there’s nothing like eyeballing a patient when giving them bad news, rather than turning away from them to scrutinise your computer screen while struggling to spell a key word or find the acronym that nobody else will understand. Dr Watson counselled us to tell the patient when you are using a scribe and asking if it’s alright with them. If they say no, do you know how to switch it off and take your own notes?
He flagged a few things that can go wrong when relying on AI scribes.
- Remember to start and stop the programme.
- If it hears a word it doesn’t understand, AI will tend to ‘fill in the gaps’ with the word it thinks should be there. This is called hallucinating.
- Remember to transfer the scribe output to your practice software.
- Try to understand how it works and the language it uses.
- How is patient privacy and confidentiality maintained? There has to be compliance with data security and privacy laws.
- How and where are the data retained? Are they encrypted?
- Where are the servers? They should be in Australasia, ie. within a jurisdiction that has sovereign laws, including Māori sovereignty.
- Has the patient given consent and do they understand what that means?
- Are there identifiable or de-identifiable data?
Ultimately, the practitioner is responsible for delivery of safe care and meeting professional obligations. The AI scribe might be intelligent, but is it intuitive? Intuition comes with experience. The parting advice from Dr Watson was “it will come your way, so embrace it and use it well to benefit your patients and your practice”.
There are currently two AI scribes in New Zealand approved for medical use and endorsed by Te Whatu Ora’s advisory group: Heidi Health and iMedX.
In the ick of it

Fig 1. Dr Tanya Trinh's slide on eye rubbing in keratoconus patients
Staying with the theme of using technology to communicate with your patients, international guest speaker Dr Tanya Trinh gave an entertaining and informative presentation on social media experts, ethics and excellence. The Australian ophthalmologist specialising in cornea, cataract and refractive surgery, has multiple fellowships, awards and published papers to her credit and is also known for her social media presence.
She commenced her talk by admitting, “If I am really honest, social media gives me the ick.” Having found it an exhausting and unhealthy addiction, she purposely locked herself out of it but now has an app to prevent her from scrolling her social media except for certain times of the day. She still maintains her own presence on various platforms as she said she doesn’t trust anyone else to maintain her high standards. Her motivation is communication and education about eyecare and what she does in her core role as an eye surgeon.
Since different platforms have different functions, it is not appropriate to spread the same message over different types, she said. Her goal is to educate colleagues, other specialists and medical practitioners and to meet patients where they are (presumably on social media!). She emphasised that her motivation is not attention seeking, which, in Australia, is closely monitored by AI scouring websites for offending medical practitioners to offer a warning and AU$50,000 fine.
She advised those wanting to enter this space to stay in their own lane by only speaking on what their area of expertise is. It requires a lot of time, as well as the financial input, to get a professional quality output. Her tips for social media novices are to have a high-quality photo library, book a high-quality local photographer, use templates to start and keep videos between 1.5 to 3 minutes long. Captions are also important and cover photos are helpful for reference. Dr Trinh also cautioned about maintaining boundaries with patients communicating via social media about their eye problems. Her final point in this space was to ask yourself whether you are adding value or just noise.
Her second lecture was about stopping cone progression in keratoconus. Dr Trinh’s experience is that patients often present with a lot of confusion about what keratoconus is. They have been given a diagnosis then discharged, never to return for follow-up. “Education is prevention,” she stated. She believes her first consultation with a potential keratoconus patient is the most important and tells them so at the start of a consultation. She explains what the cornea is and does and shows normal topography compared to a keratoconic cornea with its peaks and valleys and how a clear picture is distorted by keratoconus. Dr Trinh also discusses thinning and photographs Munson’s sign to show the patient and document changes as a cone progresses.
Dr Trinh then tackled the difficult question of what sort of eye rubber are you – a knuckler, palmer, wiper or frotter? (Fig 1). There are three reasons to rub: itchiness, dry eyes or habit. She then showed a very damning video of what happens to an eyeball as it is being rubbed. There is no social stigma to eye rubbing and it is often innocent, unconscious behaviour. A chronic rubber needs a support person to be appointed to give verbal reminders (or a kick under the table) to stop rubbing. Sometimes people don’t rub during the day, explained Dr Trinh, and allergy sufferers will rub particularly after they get out of a hot shower, which causes a histamine release.
Sleep position can have a marked effect on cone development, she said, with sleeping on the back being the least problematic. Side sleeping is acceptable only if there is nothing like a pillow crushing the eye. Stomach sleepers are most at risk, often turning their heads to the side and compressing the face on their arm, potentially deforming a vulnerable cornea. According to Dr Trinh, it takes about six months to change a sleep position and may involve use of modified pillows or sleep masks, such as those used for sleep apnoea, or a referral to the GP and/or a sleep physician.

Dr Tanya Trinh presenting
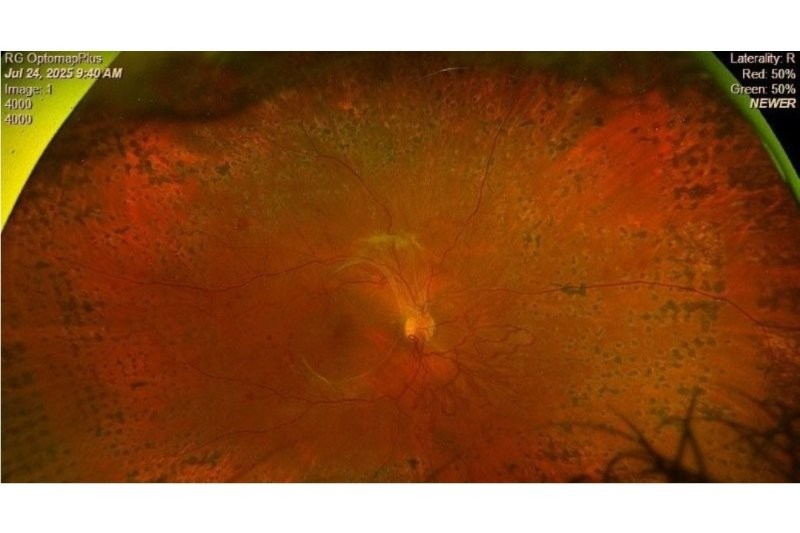
From fluids to flocks
Dr Narme Deva gave an update on treatment options for the dreaded intraretinal fluid. She maintains that OCT is the main tool for monitoring retinal conditions, since relying on best corrected acuity will flag issues far too late to consider treatment options. Where the fluid sits really matters. Serous pigment epithelial detachment depends on the underlying cause and if it’s stable. Subretinal fluid is bad, depending on how much and if it is stable; intraretinal fluid is really bad, but not all fluid indicates activity and the need for immediate action. There are a lot of nuances to fluid and knowledge of it is still evolving. The main thing is monitoring for fluctuation in fluid, as this can lead to fibrosis, which can lead to poor visual outcome and for which there is no treatment.
After morning tea, Professor Dame Helen Danesh-Meyer and Dr Kaliopy Matheos performed a duet labelled ‘The scary aspects of glaucoma – the wolf hiding among the sheep in the flock of patients in a routine day’.
The key take-home messages were:
- Monocular colour vision should be done on every new patient. Together with visual fields, these are useful screening tests for optic neuropathy.
- Binasal loss of ganglion cell layer when asymmetrical is very suspicious.
- Any patient with disc pallor who has not had acute disc swelling requires imaging.
- Where optic disc drusen are present, ocular hypertension seems to exacerbate the insidious field loss.
Dr Hannah Kersten gave an update on research, focusing on ophthalmic assessments of non-ophthalmic systemic drugs such as hydroxychloroquine, used to treat autoimmune diseases such as rheumatoid arthritis and lupus. Any part of the eye can be affected by systemic drugs, but eye people are not often part of the research team in trials of new treatments. Other events, such as rapid lowering of HbAlc glycaemic control in diabetes, can increase pre-existing retinopathy. The reason for this is not fully understood but is thought to be due to retinal vascular changes. Dr Kersten’s take-home message was to always confirm the medications your patients are taking, communicate with their specialist and GP and complete a comprehensive pre-treatment assessment to establish a baseline and plan appropriate reviews.
Dr Peter Hadden gave us a bird’s eye view of ocular trauma subtitled ‘The good, bad, ugly and unusual’. He advised us to refer if the retina can’t be seen and/or there is any fluid leakage from the globe, as seen when using fluorescein. Intraocular foreign bodies must come out unless it is an eye with no visual potential, but steel may cause a vitreous or retinal detachment, which is more urgent to fix than removing the offending object. However, the worst offenders of blunt trauma are squash balls and badminton shuttlecocks, which neatly fit within the bony orbit. Big objects like a rugby ball may break bones, but the eye is more protected. The presence of hyphaema means the eye has had a decent whack and should have urgent and ongoing ophthalmic evaluation. There may be hidden damage to the iris and/or angle, which may lead to complications such as angle recession glaucoma, corneal blood staining or re-bleeds. Shockwave force may also be projected backwards along the visual axis, affecting the lens, macula, retina and optic nerve without any immediately obvious damage.

Vicky Wang, Dr Sophie Hill, Jacqueline Ling and Wen Li Keng
Dr Sophie Hill spoke of the rising global prevalence of high myopia, which is creating an increase in cases of pathological myopia. Myopic degeneration is now a leading cause of central vision loss in working-age adults and results from structural stress of elongation, not refractive error alone.
Lacquer cracks are fine irregular yellowish lines at the posterior pole representing breaks in Bruch’s membrane. These need careful monitoring as any sudden vision distortion can indicate myopic choroidal neovascularisation (mCNV) developing along a crack. The Förster-Fuchs’ spot is a pigmented scar that forms after a mCNV lesion has regressed and healed, while mCNV is the active, initial growth of abnormal new blood vessels from the choroid into the retina. The most important factor is differentiating between a simple Förster haemorrhage, and one caused by mCNV.
Dr Hill advised the optometrist’s role is urgent identification and referral with baseline imaging, if possible. High myopes should be reviewed every 6–12 months if stable but immediately if symptoms occur. Refer to an ophthalmologist for urgent intravitreal anti-VEGF treatment if mCNV is suspected. Beyond that, offer patient education on symptoms, such as new distortion or blur, and the use of the Amsler grid for self-monitoring to report changes as soon as possible. A big tick to Dr Hill for including that low-vision rehabilitation may be required and listing this point under the role of the optometrist!
The newest face in the EI lineup is Dr Stef Guglielmetti, who initially gained his ophthalmology training in South Africa, moved on to Moorfields and subsequently acquired a fine collection of fellowships. After a 10-year stint as CEO of Johannesburg Eye Hospital, he is now enjoying sunny Northland and has recently come under the umbrella of EI in Whangārei.
Dr Guglielmetti’s topic of choice was corneal tomography. Topography, he explained, is two-dimensional, only describing the anterior surface, whereas tomography offers three-dimensional representation. Modern anterior segment OCT platforms give extremely accurate corneal tomography, which includes epithelial mapping. This is advantageous in conditions such as keratoconus, which can be masked or mimicked by other conditions. The normal epithelium is not a homogeneous layer and tends to be 5.7 micrometres thicker inferiorly due to the pressure of the upper lid. Corneal tomography with epithelial mapping describes the complete corneal structure. For example, a doughnut pattern indicates an underlying stromal cone. In conclusion, Dr Guglielmetti reminded us that an irregular topography means an irregular epithelium and that the epithelium has a refractive effect. Epithelial mapping is therefore a very helpful aid in accurate diagnosis, particularly of keratoconus.
The final presentation, from Dr Graham Reeves, was about things that look like primary open angle glaucoma but aren’t, with a review of pseudo-exfoliative glaucoma, neovascular glaucoma where VEGF is released from an ischaemic retina, and uveitic glaucoma, which is often signalled by a history of systemic disease. This warranted a well-thrashed quote: “If it looks like a duck and walks like a duck… there is probably a duck hiding in there somewhere.”

Naomi Meltzer is a retired optometrist and low vision consultant. She is a regular contributor to NZ Optics.