SPONSORED Celebrating eyecare from yesterday to tomorrow
Held at the stunning Under the Dome venue in the Auckland War Memorial Museum, Auckland Eye’s August dinner seminar was aptly themed, ‘Vision through time: honouring the past, shaping the future’.
Amid the fairy lights inside and the lights of the city outside, Dr Justin Mora thanked the evening’s sponsors, Alcon, Glaukos, i-Lumen Scientific, OptiLight and Zeiss and introduced the evening’s talks.
Auckland Eye has been in existence for 32 years, he said, during which much has changed. It now has eight locations: six in Auckland plus practices in Whangarei and Queenstown; it launched the first dedicated dry eye clinic in New Zealand; has the largest sub-specialty expertise in the country; and runs shared-care myopia clinics. Details of its dedicated referral pathway and manual, covering most ophthalmic conditions, can be found on its website, which is now available in multiple languages and in text-to-speak mode. So things certainly have changed, said Dr Mora, before introducing one of Auckland Eye’s longest-serving partners, Dr Stephen Best.

Auckland Eye choir provided mid-evening entertainment
Optic neuropathy to corneal donation substitutes
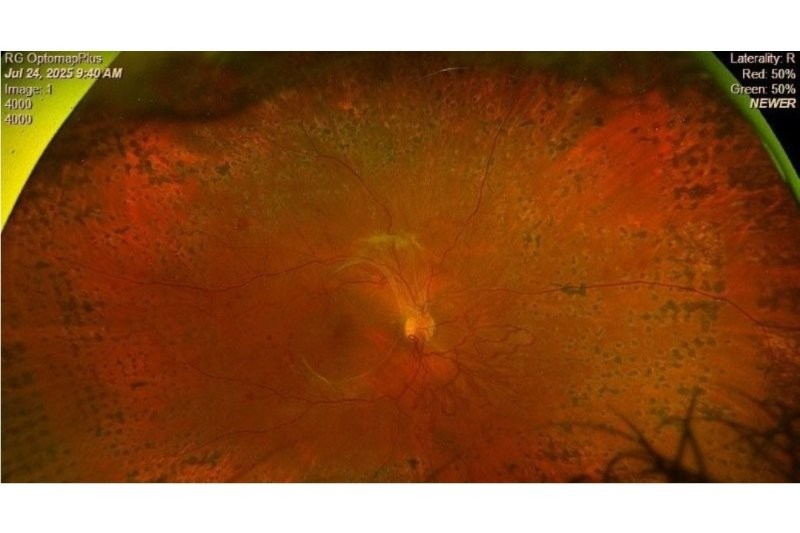
Dr Best discussed three optic nerve cases, all of a similar age but with different underlying pathologies to demonstrate diagnosis differences. Contrary to common opinion, ophthalmologists don’t order scans all the time, he said. “But when a patient has bilateral disc swelling, unusual, atypical unilateral swelling or they are in an age group where you think, ‘what else is going on?’, they need scans.”
Non-arteritic anterior ischaemic optic neuropathy (NAAION), the autoimmune inflammatory condition neuromyelitis optica spectrum disorder and optic nerve meningioma can all cause vision loss in one eye. Correct diagnosis is important as treatment and prognosis differ significantly. If a patient has sudden onset of vision loss, think vascular pathology; rapid onset, inflammatory pathology; and slow onset, compressive lesion.
Auckland Eye’s newest member, Dr Bia Kim, then tackled the increasing lack of donor corneal tissue with only one in 70 patients who need a corneal transplant currently receiving one. Help is on the horizon, however, with several synthetic alternatives in development, including artificial corneas (EndoArt, C-Clear and CorNeat); tissue-engineered corneas, including decellularised corneal scaffolds and collagen-based hydrogels; induced pluripotent stem cell-based therapies; and regenerative or gene-based therapies.
Dr Kim reminded attendees of the key signs of graft rejection, summarised by ‘RSVP’ for Redness, Sensitivity to light, Vision changes and Pain, and to refer early.
Paediatric care to breakthrough research (and a musical interlude)

Dennis Oliver and Dr Stuart Carroll
Dr Stuart Carroll discussed incomitant strabismus, where the deviation angle changes depending on the direction of gaze or which eye is used for fixation, but the eye turns are not consistent in all directions. Strabismus patients should be referred, he said, when there is a new-onset or progressive limitation of movement, suspicion of thyroid or an inflammatory cause, or the condition impacts the patient’s quality of life or binocular function.
Dr Yvonne Ng provided an overview of Auckland Eye’s myopia clinic. Running through the basics of myopia management, she discussed rapid myopia progression diagnosis and treatments, including spectacle lenses (peripheral retinal defocus lenses and Diffusion Optics Technology lenses) and myopic defocus contact lenses (orthokeratology), atropine eyedrops, repeated low-level red-light and behavioural and environmental interventions, such as increased outdoor time and reducing time spent on near tasks.
A mid-evening interlude was provided by Auckland Eye’s in-house choir, which led to much applause from the evening’s appreciative diners. This was followed by a look into the future by Dr Shenton Chew who provided an overview of several studies Auckland Eye’s research department is working on. These include:
- A clinical investigation into two Tecnis IOL models vs Eyhance (the control)
- A comparison study of Glaukos iStent Infinite latest MIGS device with other MIGS devices
- The PRISM eyedrop study for pterygium
- The Tigris trial evaluating an investigational drug-eluting IOL for cataract and glaucoma
- The Compass trial focusing on a novel, light-activated treatment for patients with ocular melanoma
- KRIYA-825, a potential one-time gene therapy for geographic atrophy
- The i-Sight2 study evaluating the i-Lumen microcurrent electrical stimulation device to slow AMD progression.
More details can be found at Auckland Eye, said Dr Chew.

Germaine Joblin, Priyal Bhoola, Jas Walia and Ammaarah Khan
Eyelid surgery through time and glaucoma today
Returning to the past, Dr Taras Papchenko provided an amusing overview of surgery throughout history. From trepanation (drilling holes in the skull) in the stone age (the oldest skull dated back 9,300 years ago) to ancient Egyptian, Indian and Roman texts describing ocular pathologies. These also included early descriptions of ptosis, entropion and ectropion repair. “A type of blepharoplasty was described by Arab surgeons in the 10th century BC involving cauterisation of excess skin,” reported Dr Papchenko, while early cosmetic surgery, particularly nose surgery, became a thing among European aristocracy in the 17th century. Throughout all, anaesthesia hardly changed at all, involving a mixture of opium and wine and henbane (nightshade) and mandrake, before diethyl ether was introduced in 1842, nitrous oxide in 1844 and chloroform in 1847. Significant advances were made in reconstructive facial surgery post-WWI, led by pioneering New Zealand-born surgeon Harold Gillies, all leading up to today’s oculoplastic sub-specialty, he said.
The last of the evening’s speakers, Dr Aaron Wong, brought the audience back to the present day with a comprehensive look at the range of current glaucoma treatment options available and the positive contribution OCT in optometry has made to early glaucoma referrals. From early referrals to MIGS and MIBS, the future is looking brighter for glaucoma patients, he said, but eyecare professionals still need to remain vigilant.