Yes sir, NOSA!
The last time I attended the Neuro-Ophthalmological Society of Australia (NOSA) meeting was in Melbourne as a first-year PhD student in 2012. I was absolutely petrified to deliver my first ever presentation to an audience composed primarily of consultant neurologists and ophthalmologists, not knowing a single person in the room. I soon realised that although it was an academically intimidating collection of people, there was a great collegial atmosphere.
I was pleased to note this friendly and collaborative environment was still present at this year’s meeting. Professor Helen Danesh-Meyer is the current president of NOSA and the first New Zealander to hold the position, so the meeting was also held in Auckland for the first time in its history. Prof Danesh-Meyer put together an exciting programme of speakers spanning a diverse range of backgrounds, including world-leading neuro-ophthalmologists from the US, UK, Australia and New Zealand, an MRI physicist, a neuropsychiatrist, research scientists, ophthalmology and neurology trainees and medical students.
The first session was opened by keynote Professor Ari Green from the University of California at San Francisco. He beautifully outlined myelin biology in multiple sclerosis (MS), pointing out that the mixture of proteins and phospholipids is one of biology’s wonders. He highlighted the importance of visual system assessment in patients with MS, particularly because close to 30% of MS patients first present with afferent visual system injury and 10–15% with efferent dysfunction. After someone has had MS for 30-plus years, the amount of axonal loss can look at least as bad as the loss seen in advanced glaucoma, but new MS therapies make a difference to how rapidly patients lose retinal nerve fibres. An interesting fact: myelination typically progresses posterior to anterior and the frontal lobe is not fully myelinated until the late teens in women and mid-20s in men!
Session two of the first day was all about idiopathic intracranial hypertension (IIH). Dr Benson Chen, a consultant neurologist and neuro-ophthalmologist at Auckland City Hospital, spoke about the condition’s expanding spectrum, ranging from IIH without papilloedema to rapidly progressing fulminant IIH. He highlighted that IIH is more than just papilloedema and headache and that the spectrum of symptoms also includes cerebrospinal fluid leak and refractory epilepsy. He also discussed glymphatic system dysfunction and its implications for the pathophysiology of IIH.

Paige Richter (the youngest presenter!) and Dr Benson Chen
Next, Professor Grant Liu from the University of Pennsylvania elegantly presented his research on IIH in the paediatric population, noting there are some key differences between paediatric and adult IIH. The latter occurs almost exclusively in obese women, whereas children and non-obese male patients can also have the disease. Abducens (sixth) nerve palsy is also more common in paediatric IIH patients, seen in about one-third of cases. I was reassured to hear that even highly experience clinicians can have difficulty discriminating a ‘full’ optic disc from papilloedema. In Prof Liu’s clinics, if a child with an elevated optic disc (query papilloedema) has a global retinal nerve fiber layer (RNFL) thickness of greater than 140µm, they get an MRI; below that threshold they are observed (although he noted there have been cases of atrophy in patients who had a starting global RNFL of less than 140µm).
The IIH session was closed by Dr Sui Wong, from London’s Moorfields and St Thomas’ hospitals, who spoke about facilitating sustainable lifestyle changes and remission through a group clinic model. She spoke about her experience in setting up group consultations for patients with IIH, developed in collaboration with the patients themselves. Patients who consented to participate in these 90-minute group sessions found them beneficial as they had more access to the healthcare team and had the opportunity to discuss challenges, including mental health hurdles, with other patients, reducing feelings of isolation. There is generally remission of IIH in patients who are able to lose 10–15% of their body weight and the idea was that this might be more likely to occur if patients had more discussion about lifestyle factors and more interaction with their patient peers.

The Vision Research Foundation crew: Jackie Low, Dr Hannah Kersten, Professor Helen Danesh-Meyer and Akarsh Mathrani
At the end of the IIH session, there was an excellent discussion about whether IIH should be renamed (again!). Prof Liu argued that IIH is a misused term as something should not be labelled ‘idiopathic’ when a causative agent can be identified (eg. with tetracycline antibiotics). Maybe we will soon see a resurgence of the term ‘pseudotumour cerebri’?
The afternoon sessions included a number of other illuminating presentations. Dr Rachael Niederer focused on the broad range of neurological sequelae of herpes zoster from cranial nerve palsies and encephalitis to neurotrophic keratopathy and post-herpetic neuralgia. She also outlined the association between herpes zoster and dementia and stroke, with antivirals showing a protective effect and the zoster vaccine reducing stroke incidence.
Professor Owen White’s talk helped to further our understanding of visual snow syndrome, a common sensory processing disorder. There are differences in fMRI imaging and saccades between controls and subjects with visual snow. I was intrigued to hear that patients with visual snow who remember their dreams do not have visual snow in their dreams!
Tales of gaze and beige
On day two, Prof Liu delivered a rapid-fire talk on the eye movement disorders we do not want to miss, including cranial nerve palsies (and mimics, such as myasthenia gravis), conjugate gaze disorders (for example Parinaud’s syndrome, where the patient is unable to look upwards), ocular motor apraxia (a deficit of saccades) and the various types of nystagmus (which should be named according to the direction of the nystagmus in the fast phase). Prof Liu succinctly explained these complex conditions and I left the session with an improved understanding of ocular motor abnormalities (and several pages of notes!).
Continuing the efferent visual system theme, Dr Wong gave her 12 top tips for the examination of patients with myasthenia gravis, a condition with hallmark variability and fatiguability. She stressed the importance of documenting the cover test and diplopia findings in all nine positions of gaze, always checking both ductions and versions, testing saccades and inactivating the frontalis muscle. Dr Wong also advocated the use of the Mestinon challenge test (aka the Tensilon test), building up the dose over six weeks and keeping a diplopia diary.
Dr Sarah Hull presented a sobering case series of four New Zealand children who had all irreversibly lost vision due to extremely low vitamin A. All of them had extremely restricted ‘beige diets’ (mostly refined carbs and low in nutrients), but did not necessarily appear malnourished. The retinal nerve fibre layer and ganglion cell layers showed significant thinning over the course of follow-up. Clinicians should be aware of the risk of nutritional optic neuropathy resulting from restricted diets, which is more common in male children and those on the autism spectrum. This rare, devastating vision loss could be avoidable.
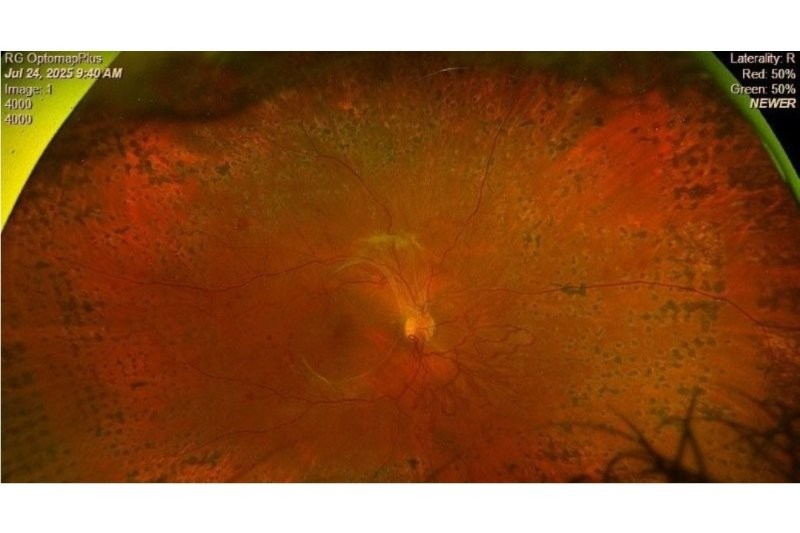
Professor Michael Barnett, the Asia-Pacific keynote speaker, eloquently outlined Susac syndrome in his talk titled ‘Big trouble in little vessels’. There is a classic triad of Susac syndrome: encephalopathy, sensorineural hearing loss and branch retinal artery occlusion. However, only 15–30% of patients have all three features at presentation. Characteristic ophthalmic findings include Gass plaques, peripheral retinal microaneurysms and arteriolar wall hyperfluorescence on fluorescein angiography.
A highlight of the conference is always the Walsh Williams Cases session (the ‘WW’ could stand for ‘weird and wonderful’). All clinical presentations were accompanied by neuro-radiological and neuropathological commentary by UNSW Sydney’s Associate Professor Yael Barnett and Auckland neuropathologist was Dr Clinton Turner. These cases are often once- or twice-in-a-career diagnoses and this year included the rare blood disorder, Erdheim-Chester disease (which had a pathognomonic finding of hairy kidneys), lymphocytosis in a patient with a history of IIH (the most simple answer is not always the correct one), bilateral sequential central retinal artery occlusion (incidence of approximately 1 in 5 million) and the elegantly named POEMS (polyneuropathy, organomegaly, endocrinopathy, myeloma protein and skin changes) syndrome (another rare blood disorder, in which the disc oedema is thought to be due to elevated VEGF and increased vascular permeability). There was insightful audience participation and all presenters spoke with passion and enthusiasm. For me, the take-home message from this session was, when you are confronted with an overwhelming case, go back to basics and write down what you know to be true.
The conference was closed by Prof Green, highlighting the clinical trials in remyelination, the holy grail of MS treatment. Patients in remyelination trials must be on immunosuppressant therapy, otherwise it is like rebuilding a house that is still on fire, he said. There are big questions to be answered, including how to measure myelin restoration and how to assess whether a new drug is effective (electrophysiology may be useful).
It felt like a fitting conclusion to such an enjoyable and stimulating two days. I learned so much and it was amazing to hear from such a variety of internationally renowned speakers. It definitely won’t be another 13 years before I attend the next NOSA meeting!

Dr Hannah Kersten is the research manager at Eye Institute and continues to work as an optometrist, with a particular interest in neuro-ophthalmic disease and glaucoma. She is a trustee of Glaucoma New Zealand and Vision Research Foundation.