Ophthalmology, the future and beyond: opportunities and challenges for humanity
The ophthalmology odyssey is a story of discovery and great achievement, especially with the advent of modern technological advancements and progress in surgical techniques and treatment of blinding disease. In the 1960s, phacoemulsification was pioneered by visionary ophthalmologist Dr Charles Kelman as a novel technique for performing cataract surgery1. Recently, ophthalmic innovations such as optical coherence tomography (OCT)² have been a boon in enabling eyecare professionals to diagnose ocular pathology, while intravitreal anti-VEGF medications, introduced in 2002 for the treatment of age-related macular degeneration (AMD), have revolutionised retinal disease management3. Nanotechnology, bionic retinal implants, gene therapy and stem cell treatments are other contemporary developments in this visual-sciences journey, each introduced with varying levels of success.
A great limitation with many new treatments, however, is the ability to demonstrate robust evidence for their efficacy in long-term follow-up studies. For example, N-acetylcarnosine was touted as a prophylactic eye drop in cataractogenesis, but further studies are yet to substantiate these claims4. As such, eyecare professionals must consider the judicious balance between early adoption of treatments versus waiting for confirmatory evidence.
Lifestyle adaptations
Cataract, AMD, glaucoma and diabetic retinopathy are expected to increase in the future as humans age and approach ‘longevity escape velocity’ (where medical advances extend human lifespans by more than their expected lifespan at birth) and thus become increasingly comorbid5. Implementing practical measures, such as adjusting workplace practices, can significantly impact overall health, for example by mitigating cardiovascular risks linked to prolonged sedentary behaviour6. Sitting is an independent risk factor for cardiovascular comorbidity, which may also be directly associated with eye disease6. Systemic disease can have a multitude of ocular manifestations, while lower physical activity levels are associated with glaucoma, AMD, diabetic retinopathy and retinal vascular diseases7. Thus, lifestyle modifications, preventative eyecare and workforce changes are critical public health initiatives and a starting point for change.
Telemedicine and extended reality technology
Teleophthalmology is a rapidly expanding field of ophthalmology that enables the delivery of eyecare via multiple digital media modalities, thereby improving patient access8. With technological improvements, smartphone fundus photography has the potential to diagnose and direct the management of conditions such as diabetic retinopathy, retinopathy of prematurity and other retinal vascular diseases9. At-home contact-lens-based intraocular pressure (IOP) measuring devices could provide real-time 24-hour data, although its current iteration may be too cost prohibitive for use as a remote screening tool10. Use of at-home OCT is also gaining validation as a monitoring tool for retinal diseases11.
Although teleophthalmology offers great potential for improving access to care by extending services to remote or under-served areas, it also poses challenges and risks. Socioeconomic disparities in access to technology and internet connectivity may contribute to the ‘digital divide’ and thus exclusion for some, thereby exacerbating existing healthcare disparities12. Transmitting sensitive medical information over digital platforms also poses privacy and security concerns. Safeguarding patient data against breaches and ensuring compliance with healthcare regulators are crucial aspects in implementing teletechnology13.
Virtual reality (VR) and augmented reality (AR) are at the forefront of technological application in ophthalmology. VR uses computerised simulation environments, whereas AR overlays virtual elements upon the real-life graphical environment14. These technologies are already employed for surgical skills training, ophthalmoscopy, visual assessment and visual-field testing14. It is plausible that future application of these technologies could extend to remote-centre clinical training, clinical assessment and diagnosis, and integrated into teleophthalmology services.
Global warming, pandemics and sustainability
A nexus relevant to ophthalmology is the anticipated increase in pandemia frequency, a concern compounded by anthropogenic climate change15. During the recent Covid-19 pandemic, there was extensive reporting of ocular manifestations, from keratoconjunctivitis to uveitis and retinal vascular disease16. Ebola can cause sight-threatening panuveitis16, raising legitimate fears that if transmission were to occur through aerosolisation, it could trigger an international humanitarian crisis17.
A negative medical externality is the cost associated with an entity’s activity that impacts others who did not choose to incur that cost. For example, products developed by the medical equipment industry create pollution, by-products and medical waste, all of which impose a cost to society and the environment. This is a pressing global issue as medical packaging waste continues to create a growing, perhaps insurmountable, ecological footprint. Sustainability policies need to balance waste minimisation with quality and sterility standards to ensure patient safety18. Climate change and the recent Covid-19 pandemic is forcing a re-think in how we approach these issues by improving the efficiency of services and sterilisation methods and the uptake of medical recyclables.
Social media and cosmetic ophthalmology
Health education and networking via social media is an increasingly important forum for ophthalmology. Social media serves as a dynamic platform for eyecare professionals to effectively share ophthalmic knowledge with the public via engagement in easily digestible formats, such as images, videos, infographics and live question-and-answer sessions19. The rapid dissemination of information on social media also poses risks, however, including the spread of misinformation and misconceptions about eye health and treatment options19. Eyecare professionals, being aware that patients may circumvent official sources of information, should learn how best to use social media to better educate and inform them accurately.
Cosmeceuticals (the combination of cosmetics and pharmaceuticals designed to access and act on the deeper layers of the skin) and aesthetic ophthalmology are growing trends with potentially deleterious outcomes. A cautionary tale came with the advent of scleral tattooing, delivering short-term popularity despite well-publicised risks of vision and eye loss20. An apparent change in eye colour may well be on the horizon via genetic engineering, yet currently available techniques, such as iris implants and keratopigmentation, come with well-established risks21. The eyecare community must continue to protect the public against procedures that do not improve vision and may cause harm, while being aware of the demand for beautification and enhancement services.
Machines in ophthalmology
There is a plethora of literature pertaining to artificial intelligence (AI) and deep learning (DL) in ophthalmology. In particular, various studies have examined its role in assessing fundus photography, OCT and visual fields for conditions including diabetic retinopathy, AMD, glaucoma, cataract, macular oedema and retinopathy of prematurity22. It is conceivable that AI will reach the ability to diagnose and manage ocular pathology independent of human input. This raises many questions regarding ethics, information storage and workforce employment, as AI displaces traditional eyecare-service models, and serves as a reminder that eyecare professionals should be involved in its future direction and functionality.
Robotic three-dimensional (3D) printing is a burgeoning field of biomaterial provision in ophthalmology, with the potential for corneal tissue bioprinting, contact lens production, drug-eluting glaucoma implants and macular buckles23. Cyber-surgery is also now possible with the advent of advanced robotic surgical tools which can reduce surgical times, perform surgery remotely and eliminate tissue trauma in delicate procedures such as epimacular membranectomy24,25. The expectation is that AI and autonomous robots will one day outperform humans in medical and surgical tasks in ophthalmology. Worker obsolescence and safety concerns regarding this technology are problems that will need to be carefully navigated, especially in these incipient automation stages.
Anti-ageing treatments
Anti-ageing therapies (senolytics) are heralded as the next transformative breakthrough in degenerative disease which will not only promote longevity but reduce cellular attrition seen with many ocular conditions. Ageing is a complex, pre-programmed process and targeting different aspects of this forms the basis of senotherapeutics (Table 1)26. The premise is simple yet elegant: delay cellular senescence and therefore delay the onset of degenerative eye disease. Theoretically, cellular immortality would eliminate degenerative eye disease altogether. It represents a major advancement from previous anti-ageing strategies achieved by calorie deprivation and intermittent fasting27. Supplements which target cellular senescence pathways are common in anti-ageing protocols; some contain agents which affect cell metabolism via mTOR, AMPK and SIRT28. Nutraceuticals such as nicotinamide mononucleotide (NMN), related to vitamin B3, have also shown promise in retarding the ageing process; however, safety concerns remain and there is a growing call for further clinical investigation with longitudinal data to affirm its efficacy28.
The human microbiome has a key immunomodulatory role in geroscience. There is evidence that focusing on a prebiotic diet with probiotic supplementation can attenuate cellular degradative processes29. Furthermore, vitamin D has multiple effects on physiological systems with recent studies highlighting its potential in delaying cellular ageing30.
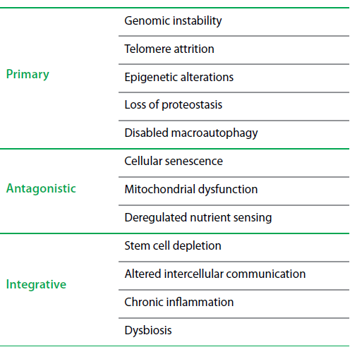
Table 1. The twelve Hallmarks of ageing
Astro-ophthalmology
Terraformation of Mars and colonisation of the Moon are possibilities only once imagined and could be detrimental to naïve eyes. The long-term effects of cosmic radiation on vision are relatively unknown but the visual disturbances perceived by astronauts, known as ‘phosphene phenomena’, have been attributed to this. The microgravitational atmosphere of these celestial bodies and interplanetary space travel itself can cause optic nerve oedema, choroidopathy and retinal microcirculatory injury – as seen in space-associated neuro-ocular syndrome (SANS)33. Adaptation pressures may change ocular anatomy, physiology and even pathology in these new environments. As space missions increase in duration and distance, further research is needed to deepen our understanding of SANS and other ocular conditions and develop effective countermeasures34.
Conclusion
The future of ophthalmology offers a multitude of possibilities as technology advances. Accessibility, cost effectiveness, safety, efficacy, feasibility, ethical, medicolegal and proprietary considerations are all important factors to be considered and a significant challenge will be ensuring these advances do not drive further health inequities, particularly within disadvantaged communities. Vocational obsolescence is another concern, with the potential for societal unrest and discord between humans and machines due to mass unemployment. Eyecare professionals will need to participate in all levels of clinical governance and political advocacy to ensure that future technology continues to serve humanity with the purpose it was intended for.
References:
- Kelman CD. Phaco-emulsification and aspiration: a new technique of cataract removal: a preliminary report. Am J Ophthalmol. 1967; 64 (1): 23-35.
- Tearny G, Boppart SA, Bouma B, Brezinski ME, Swanson EA, Fujimoto JG, inventors; Massachusetts Institute of Technology, assignee. Method and apparatus for performing optical measurements using a fiber optical imaging guidewire, catheter or endoscope. United States Patent 6,134,003 A. October 17, 2000.
- Whitescarver TD, Hobbs SD, Wade CI et al. A history of anti-VEGF inhibitors in the ophthalmic literature: A bioliographic review. J Vitreoretin Dis. Dec 2020; 5 (4): 304-312.
- Babizhayev MA, Burke L, Micans P, Richer SP. N-Acetylcarnosine sustained drug delivery eye drops to control the signs of ageless vision: glare sensitivity, cataract amelioration and quality of vision currently available treatment for the challenging 50,000-patient population. Clin Interv Aging. 2009; 4:31-50.
- Klein R, Klein BE. The prevalence of age-related eye diseases and visual impairment in ageing: current estimates. Invest Ophthalmol Vis Sci. Dec 2013; 54 (14): ORSF5-ORSF13.
- Stamakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. Apr 2019 30;73(16): 2062-2072.
- Ong SR, Crowston JG, Loprinzi PD, Ramulu PY. Physical activity, visual impairment and eye disease. Eye (Lond). Aug 2018; 32(8):1296-1303.
- Sreelatha OK, Sathyamangalam VSR. Teleophthalmology: improving patient outcomes? Clin Ophthalmol 2016; 10: 285-295.
- Iqbal U. Smartphone fundus photography: a narrative review. Int J Retin Vitr 2021; 7:44.
- Dunbar GE, Bailey YS, Aref AA. The sensimed triggerfish contact lens sensor: efficacy, safety, and patient perspectives. Clin Ophthalmol 2017; 11: 875-882.
- Liu Y, Holekamp NM, Heier JS. Prospective, Longitudinal Study: Daily self-imaging with home OCT for neovascular age-related macular degeneration. Ophthalmol Retina 2022 Jul;6 (7): 575-585.
- Scanzera AC, Kim SJ, Paul Chan RV. Teleophthalmology and the digital divide: inequities highlighted by the COVID-19 pandemic. Eye Lond Engl. 2021;35(6):1529-1531.
- Hall JL, McGraw D. For Telehealth To Succeed, Privacy And Security Risks Must Be Identified And Addressed. Health Aff (Millwood). 2014;33(2):216-221.
- Iskander M, Ogunsola T, Ramachandran R, McGowan R, Al-Aswad LA. Virtual Reality and Augmented Reality in Ophthalmology: A Contemporary Prospective. Asia Pac J Ophthalmol (Phila). 2021;10(3):244-252.
- De Oliveira T, Tegally H. Will climate change amplify epidemics and give rise to pandemics? Science Aug 2023 25;381(6660):eadk4500.
- Taha MJJ, Abuawwad MT, Alrubasy WA, Sameer SK, Alsafi T, Al-Bustanji Y, Abu-Ismail L, Nashwam AJ. Ocular manifestations of recent viral pandemics: A literature review. Front Med (Lausanne) 2022; 9: 1011335.
- Clark C. If Ebola were to become airbone, it would be a global catastrophetrophe. Nurs Stand Oct 2014 13;29 (6): 33.
- Janik-Karpinska E, Brancaleoni R, Niemcewicz M, Wojtas W, Foco M, Podogrocki M, Bijak M. Healthcare waste – a serious problem for global health. Healthcare (Basel) Jan 2023 13;11 (2): 242.
- Nguyen AAK, Tsui E, Smith JR. Social media and ophthalmology: A review. Clin Exp Ophthalmol May 2022;50(4): 449-458.
- Hida S, Chiambaretta F, Malecaze J. Scleral tattooing: A dangerous fashion trend. J Fr Ophthalmol Jun 2022; 45(6): 608-611
- D’Oria F, Abu-Mustafa SK, Alio JL. Cosmetic change of the apparent color of the eye: A review on surgical alternatives, outcomes and complications. Ophthalmol Ther Apr 2022; 11(2): 465-477.
- Ting DSW, Pasquale LR, Peng L, Campbell JP, Lee AY, Raman R, Siew G, Tan W, Schmetterer L, Keane PA, Wong TY. Artificial intelligence and deep learning in ophthalmology. Br J Ophthalmol Feb 2019;103 (2): 167-175.
- Tan G, Ioannou N, Mathew E, Tagalakis AD, Lamprou DA, Yu-Wai-Man C. 3D printing in ophthalmology: from medical implants to personalized medicine. Inj J Pharm Sep 2022 25;625: 122094.
- Pandey SK, Sharma V. Robotics and ophthalmology: are we there yet? Indian J Ophthalmol Jul 2019; 67(7): 988-994.
- Turgut F, Somfai GM, Heussen FM, Eberle A, de Smet MD, Becker MD. Robot-assisted epiretinal membrane peeling: a prospective assessment of pre- and intra-operative times and of surgeon’s subjective perceptions. J Clin Med Apr 2023; 12(8): 2768.
- Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: An expanding universe. Cell Jan 2023 19;186 (2): 243-278.
- Shetty AK, Kodali M, Upadhya R, Madhu LN. Emerging anti-ageing strategies – scientific basis and efficacy. Aging Dis Dec 2018; 9(6): 1165-1184.
- Nadeeshani H, Li J, Ying T, Zhang B, Lu J. Nicotinamide mononucleotide (NMN) as an anti-aging health product – Promises and safety concerns. J Adv Res. 2021 Aug 11;37:267-278.
- Boyajian JL, Ghebretatios M, Schaly S, Islam P, Prakash S. Microbiome and human aging: probiotic and prebiotic potentials in longevity, skin health and cellular senescence. Nutrients. 2021 Dec 18; 13 (12): 4550.
- Sosa-Diaz E, Hernandez-Cruz EY, Pedraza-Chaverri J. The role of vitamin D on redox regulation and cellular senescence. Free Radic Biol Med. 2022 Nov 20;193 (Pt 1): 253-273.
- Aleci C. From international ophthalmology to space ophthalmology: the threats to vision on the way to Moon and Mars colonization. Int Ophthalmol. 2020 Mar;40(3):775-786.
- Krittanawong C, Singh NK, Scheuring RA, Urquieta E, Bershad EM, Macaulay TR, Kaplin S, Dunn C, Kry SF, Russomano T, Shepanek M, Stowe RP, Kirkpatrick AW, Broderick TJ, Sibonga JD, Lee AG, Crucian BE. Human Health during Space Travel: State-of-the-Art Review. Cells. 2022;12(1):40.
Dr Eugene Michael is a medical and surgical retina fellow at the University of Alberta, Canada. He completed his medical school and ophthalmology vocational training in Auckland, New Zealand.
Angie Hu is a medical student at the University of Alberta with an interest in AI technologies.